One cold night in winter of 2003 I was Chief Resident @RCHMelbourne & I was asked to give a talk to potential paed residents...there were also some of that year's residents & Director of Physician Training @margot_nash pushed them: "surely there's some bad things about paeds?" 
One particularly great resident - who had gone on to amazing things and just completed his PhD- talked about how much he loved the job but he said:
"I do drive to work each day and know I hurt children"
That changed the course of my career.
"I do drive to work each day and know I hurt children"
That changed the course of my career.
He was right.
In 2003 that was still the elephant in the room of paediatrics.
In the years that followed a huge amount of work happened around the world.
And in Australia we had the RACP guideline statement on proc pain:
racp.edu.au/docs/default-s…
In 2003 that was still the elephant in the room of paediatrics.
In the years that followed a huge amount of work happened around the world.
And in Australia we had the RACP guideline statement on proc pain:
racp.edu.au/docs/default-s…

And at RCH we did a huge amount of work. There were some amazing clinicians & leaders.
I was very lucky to be awarded a Winston Churchill Trust Fellowship @ChurchillTrust to study paediatric pain centres overseas & did pain training with FPMANZCA
I was very lucky to be awarded a Winston Churchill Trust Fellowship @ChurchillTrust to study paediatric pain centres overseas & did pain training with FPMANZCA
But most of all we did a big implementation project at RCH to improve how we cared for kids.
We called this Comfort Kids
rch.org.au/comfortkids/
And in Rheumatology we've got a heap of resources at
rch.org.au/rheumatology
And a joint injection video
rch.org.au/be-positive/#a…
We called this Comfort Kids
rch.org.au/comfortkids/
And in Rheumatology we've got a heap of resources at
rch.org.au/rheumatology
And a joint injection video
rch.org.au/be-positive/#a…

A few weeks ago I did a session with this year's residents and it made me think of that winter's night and the elephant in the room.
But also that when we started there was such a long way to go:
But also that when we started there was such a long way to go:

We discussed the need to get it right all the time.
To avoid the "Just do it" mentality.
And to see this procedure as one in a potential line of procedures for this child.
I've imagined this as a snakes and ladders board.
To avoid the "Just do it" mentality.
And to see this procedure as one in a potential line of procedures for this child.
I've imagined this as a snakes and ladders board.

We always start by a few minutes of the residents thinking about procedures that have gone well and not so well for them...
Then I write those up onto a white board.
Always fascinating, themes the same.
Eg location, parents as coaches or distressed, timing, right people...
Then I write those up onto a white board.
Always fascinating, themes the same.
Eg location, parents as coaches or distressed, timing, right people...
So...we know the evidence.
But like many areas of medicine the uptake was limited.
It's a lot better now.
There are still gaps.
But like many areas of medicine the uptake was limited.
It's a lot better now.
There are still gaps.

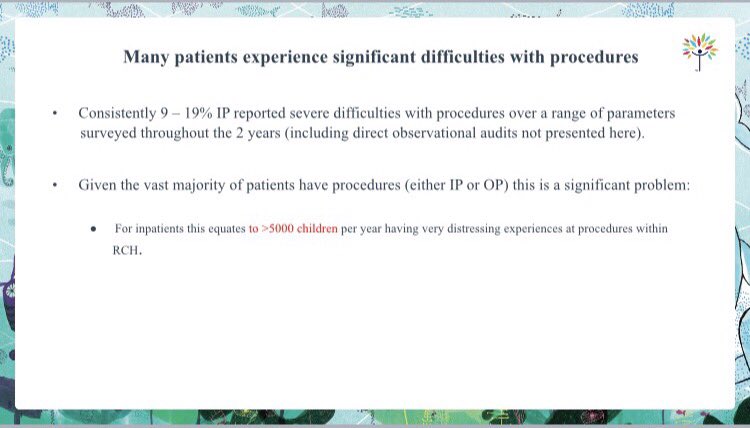
Over a number of timepoints (noting this is old data) we found a pretty large number of children - and this was consistent over time (different children, similar numbers) - who had pain and distress at procedures.
We also focussed on this group.
We also focussed on this group.
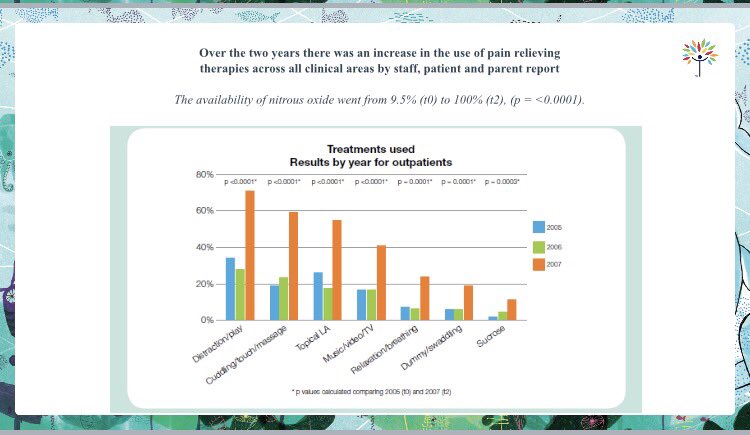
And we worked on delivering non-pharmacological and pharmacological solutions to procedural pain management for kids. 

We got some great initial results and were able to integrate education into the inpatient and outpatient settings. 
We get the residents to think about individualising combining the two approaches for each child - and asking their parents and the child what works for them. 

And tried to focus on things like
Busy Brains
Breathing
Positioning for comfort
One Voice
Parents as coaches
Sucrose
Anticipation
Preparation
Get them to make a Comfort Plan
Everyone has a role at the procedure
Busy Brains
Breathing
Positioning for comfort
One Voice
Parents as coaches
Sucrose
Anticipation
Preparation
Get them to make a Comfort Plan
Everyone has a role at the procedure

I like to think that this is our core business in getting this right for paediatrics given we do a lot of procedures on babies & kids & teens.
We've come such a long way, it's not perfect yet, but great to reflect.
We've come such a long way, it's not perfect yet, but great to reflect.
Thinking about paeds across the lifespan and setting babes and kids up for success...and not trauma and needle phobia and avoiding healthcare.
@RCHAnaesthesia @DFTBubbles @JudkinsSimon @NoNeedlessPain @DrCChambers @dharrisonCHEO @EMManchester @catherinecrock @Joshuawolf
@RCHAnaesthesia @DFTBubbles @JudkinsSimon @NoNeedlessPain @DrCChambers @dharrisonCHEO @EMManchester @catherinecrock @Joshuawolf

#ItDoesntHaveToHurt #proceduralpainmanagement
#kidspain @ANZCA_FPM @TheRACP @MJA_Editor @JPCHonline @andrewjtagg
#kidspain @ANZCA_FPM @TheRACP @MJA_Editor @JPCHonline @andrewjtagg
• • •
Missing some Tweet in this thread? You can try to
force a refresh
















