So I've been doing a bit of reading on malignant hyperthermia (MH) and learned a few things.
Here are some interesting facts on MH, presented in no particular order...
Here are some interesting facts on MH, presented in no particular order...
Most patients who suffer MH have had prior uneventful anaesthetics. In fact, in most cases the patient had 2 or more uneventful anaesthetics previously!!
ncbi.nlm.nih.gov/pubmed/20081135
ncbi.nlm.nih.gov/pubmed/20081135
Suxamethonium with volatile anaesthetic seems to be a potent trigger for MH. The relative risk of MH when using sux plus vapour is 19.6 compared to vapour alone.😬
ncbi.nlm.nih.gov/pubmed/23223104
ncbi.nlm.nih.gov/pubmed/23223104
Some have doubted that suxamethonium alone can trigger MH, but it absolutely can! The Canadians found 20 cases of sux-induced MH, all proven with muscle biopsy.
(25% occurred in ECT or ER so even trace volatile isn't an explanation.)
ncbi.nlm.nih.gov/pubmed/23842196
(25% occurred in ECT or ER so even trace volatile isn't an explanation.)
ncbi.nlm.nih.gov/pubmed/23842196
MH sux [see what I did there!], but not as much as it used to.
Dantrolene is credited for reducing mortality from ~80% to 1-2%. In fact, in the original study the treatment group had a mortality of 0%, and the delayed group 75%!!
ncbi.nlm.nih.gov/pubmed/7039419
Dantrolene is credited for reducing mortality from ~80% to 1-2%. In fact, in the original study the treatment group had a mortality of 0%, and the delayed group 75%!!
ncbi.nlm.nih.gov/pubmed/7039419
There’s no maximum dose of dantrolene according to most guidelines, but if things aren’t getting better after 10mg/kg, reconsider the diagnosis.
This paper identified one patient who received 6,860mg (100mg/kg)!!
ncbi.nlm.nih.gov/pubmed/20081135
This paper identified one patient who received 6,860mg (100mg/kg)!!
ncbi.nlm.nih.gov/pubmed/20081135

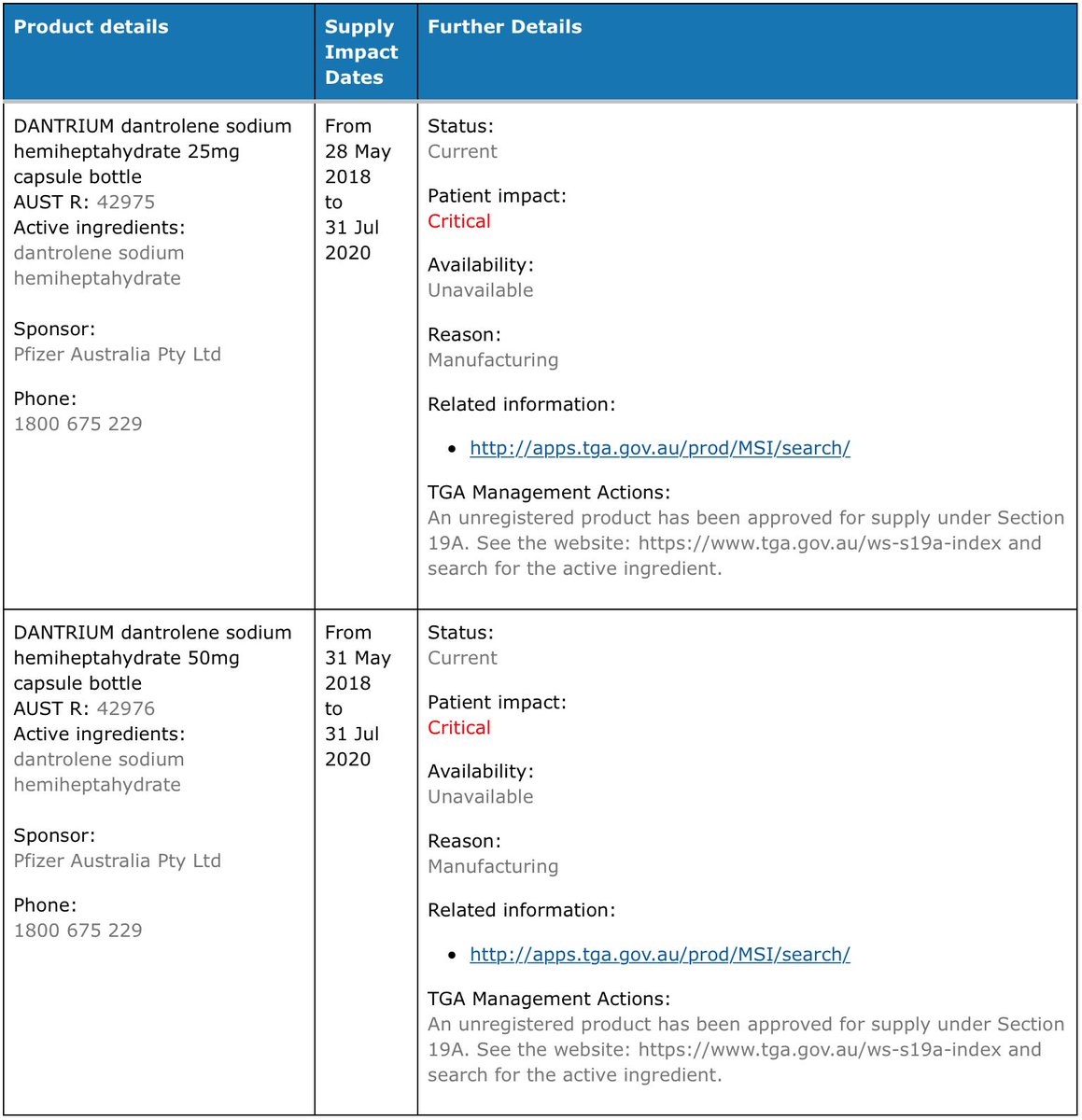
“Dantrium” 20mg ampoules are the only approved dantrolene in Australia; however you may find 25mg, 50mg or 250mg on your trolley. TGA exemptions for import are granted in times of shortage and these products hang around on the trolleys.
apps.tga.gov.au/Prod/msi/Searc…
apps.tga.gov.au/Prod/msi/Searc…
Contrary to common wisdom, increased body temperature is often an early sign of MH. In 63% of cases, hyperthermia was one of the first three signs to appear, and in 4% it was the singular first sign of the crisis.
ncbi.nlm.nih.gov/pubmed/20081135
ncbi.nlm.nih.gov/pubmed/20081135
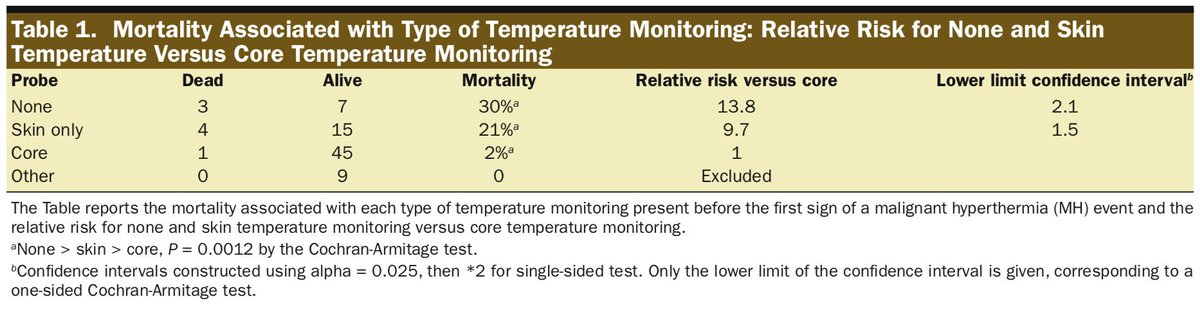
Whether a patient had core body temperature monitoring seems to be a strong predictor of mortality. Some have advocated that core temperature should be required for every GA lasting >30 minutes.
ncbi.nlm.nih.gov/pubmed/25268394
ncbi.nlm.nih.gov/pubmed/25268394
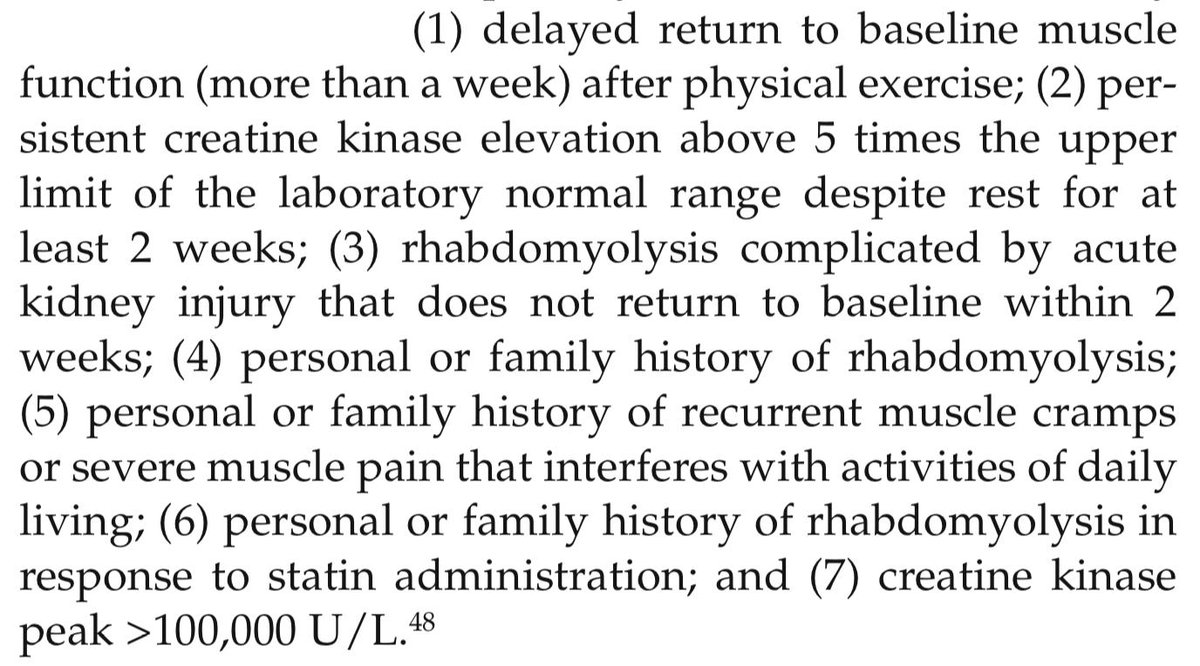
There’s some ill-defined link between MH and a heat/exercise-induced MH-like illness.
Hx of exercise/heat-induced muscle cramps / rhabdo / heat stroke may increase risk of MH, but no-one really knows what to do next. Some factors may help to stratify risk:
insights.ovid.com/crossref?an=00…
Hx of exercise/heat-induced muscle cramps / rhabdo / heat stroke may increase risk of MH, but no-one really knows what to do next. Some factors may help to stratify risk:
insights.ovid.com/crossref?an=00…
Similarly, MH-susceptible pts may suffer heat/exercise-induced illness which resembles MH (sometimes called “awake-MH”) and can be fatal.
It’s not clear how to counsel these patients, but their coaches etc should probably be made aware of symptoms.
mhaus.org/patients-and-f…
It’s not clear how to counsel these patients, but their coaches etc should probably be made aware of symptoms.
mhaus.org/patients-and-f…
OK; final fact:
You may already know that the first known survival from MH was at @TheRMH by Dr James Villiers in 1960. Pt was a 21-year-old with a compound fracture post MVA; 10 family members had already died of unknown cause while under GA!!
But what you may not know is...
You may already know that the first known survival from MH was at @TheRMH by Dr James Villiers in 1960. Pt was a 21-year-old with a compound fracture post MVA; 10 family members had already died of unknown cause while under GA!!
But what you may not know is...
The GP was also well-aware of the pt's family Hx. So much so that when as a 12-year-old he needed an appendicectomy, the GP performed it under local anaesthetic.
That's right- the GP did an appendicectomy on a 12-year-old under local!!
That's all, tweeps.
anesthesiology.pubs.asahq.org/article.aspx?a…
That's right- the GP did an appendicectomy on a 12-year-old under local!!
That's all, tweeps.
anesthesiology.pubs.asahq.org/article.aspx?a…
• • •
Missing some Tweet in this thread? You can try to
force a refresh