For the next 2 weeks @PBM_NHS are focussing on O D neg. I’ve got a few #tweetorials up my sleeve; but why is O D neg so important? Can I convince you to make focussing on saving this #preciousblood your #Onegoal for the fortnight? #blooducation
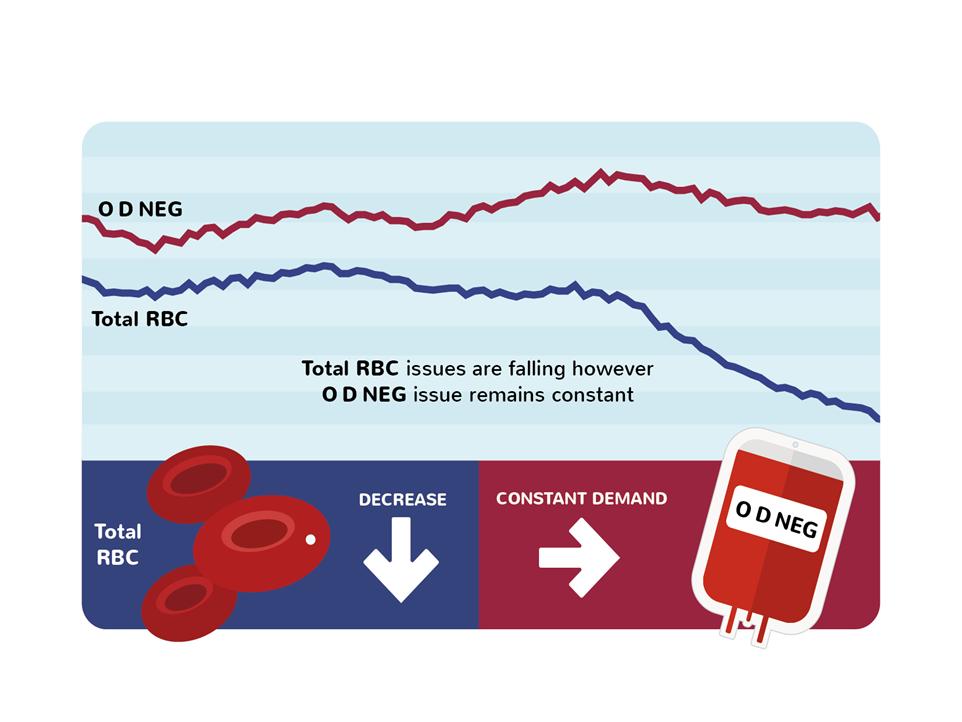
@PBM_NHS Overall red cell issues are falling but O D neg use is static/rising due to increased survival of trauma patients to hospital and increased complexity of transplantation – this is a good thing! But as a %, O D neg use is going up. 
@PBM_NHS O D neg people comprise 7% of both patient and donor population; O D neg patients need O D neg blood, and other key patient groups too (more on that later), so we are always needing to ask more of our O neg donors than others.
@PBM_NHS We think of “O neg” as being “universal” blood but this is flawed for 2 reasons
1.No red cells can be considered compatible until an antibody screen has been performed
1/2
1.No red cells can be considered compatible until an antibody screen has been performed
1/2
@PBM_NHS 2. Group O and D neg are actually two distinct requirements; group O avoids ABO incompatible transfusion; D neg avoids alloimmunisation of D neg patients against the D antigen
@PBM_NHS *question time*
Can the #haemSpRs (and others!) give some indications for times when group O blood is required?
Can the #haemSpRs (and others!) give some indications for times when group O blood is required?
• • •
Missing some Tweet in this thread? You can try to
force a refresh




