You’re going to hear a lot about red meat tomorrow. @AnnalsofIM has published 4 SRs & recommendation from Gordon Guyatt & others.
Here was my take for @SMC_London
And an old thread that is relevant here.
Here was my take for @SMC_London
And an old thread that is relevant here.
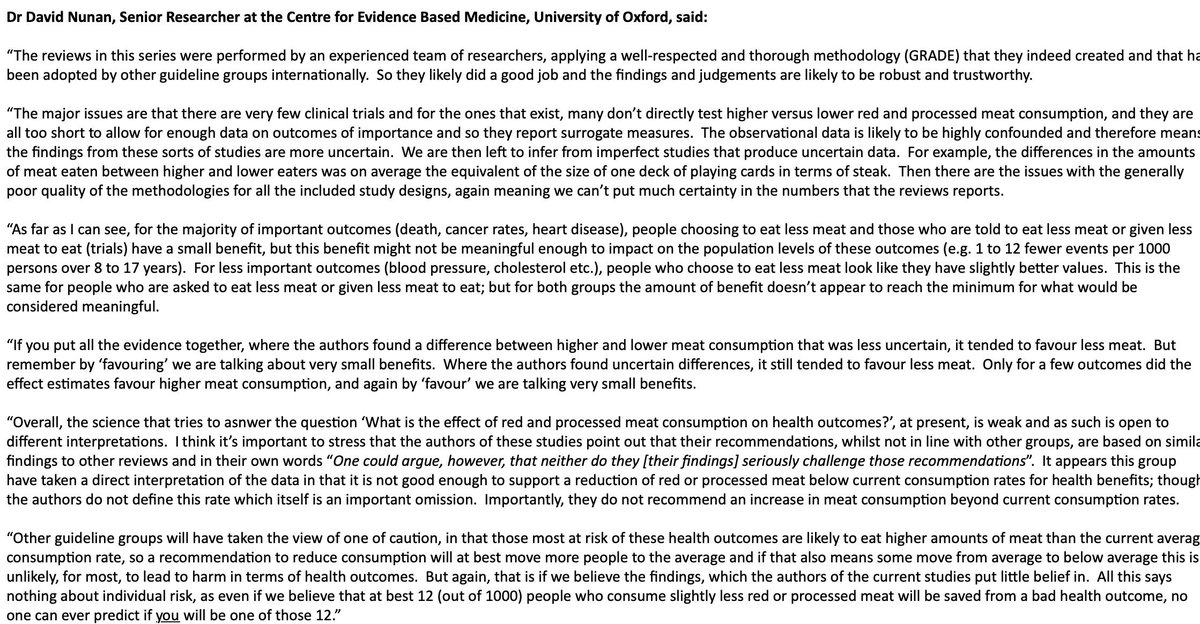
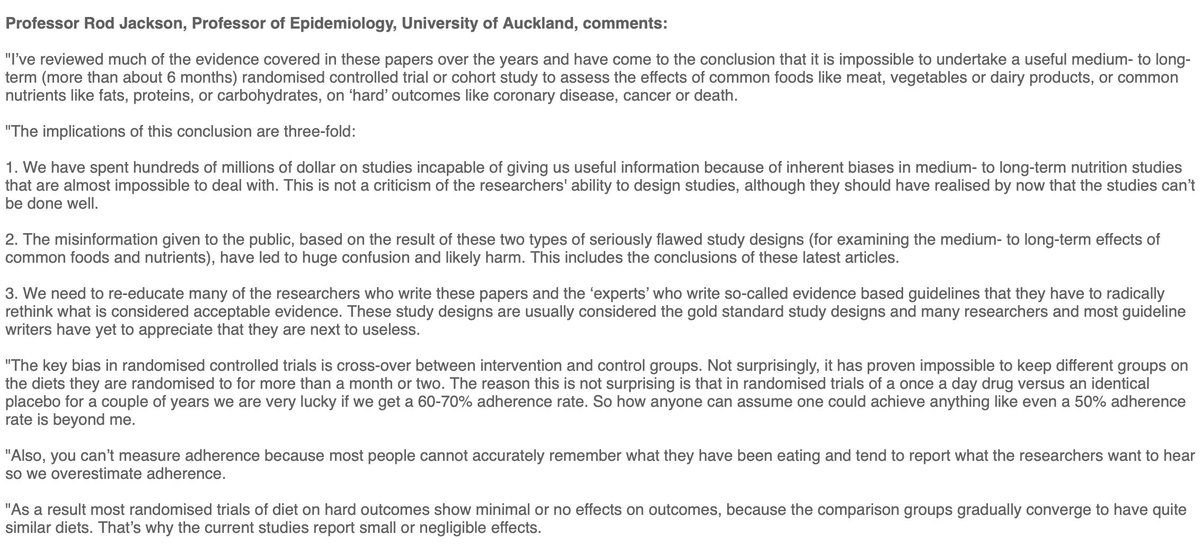
@AnnalsofIM @SMC_London Also, folk might like to see the reactions of other ‘experts’ here:
https://twitter.com/SMC_London/status/1178792460266422277
Let’s not forget that the latest #redmeat studies do not recommend eating MORE meat!
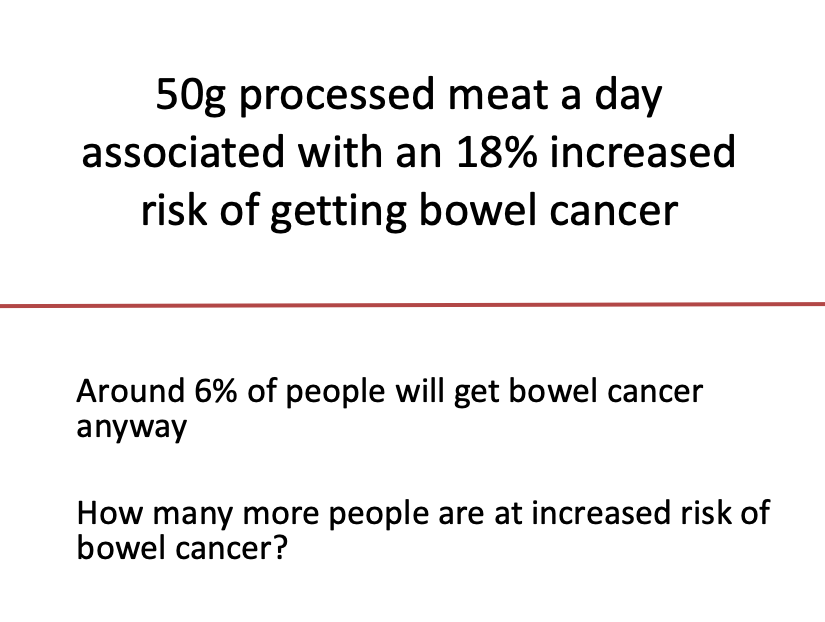
They just don’t have much confidence in the evidence they reviewed that underpins the observed small increased risk with eating 3-4+ servings per week.
They just don’t have much confidence in the evidence they reviewed that underpins the observed small increased risk with eating 3-4+ servings per week.
Just realised could have phrased some things a bit better.
When I (& others) say “small benefits”, what we mean is that only a few people (out of many, say 1000) see the benefit. That’s not to say that the health outcome(s) that benefit are not important, especially to you.
When I (& others) say “small benefits”, what we mean is that only a few people (out of many, say 1000) see the benefit. That’s not to say that the health outcome(s) that benefit are not important, especially to you.
• • •
Missing some Tweet in this thread? You can try to
force a refresh