First up, I presented the National Comparative Audit of transfusion associated circulatory overload. There is more to TACO than perhaps meets the eye; good
review article here onlinelibrary.wiley.com/doi/full/10.11…
review article here onlinelibrary.wiley.com/doi/full/10.11…
ISBT revised the definition of TACO in March 2019 (which remains a clinical diagnosis) - paper is here
isbtweb.org/fileadmin/user…
isbtweb.org/fileadmin/user…
Onset during or up to 12 hours after transfusion (SHOT up to 24h)
≥1 required criterion AND ≥3 criteria i.e. A and/or B, and total of at least 3 of A to E
Required criteria
A. Acute or worsening respiratory compromise
B. Evidence of acute or worsening pulmonary oedema 1/
≥1 required criterion AND ≥3 criteria i.e. A and/or B, and total of at least 3 of A to E
Required criteria
A. Acute or worsening respiratory compromise
B. Evidence of acute or worsening pulmonary oedema 1/
Additional criteria
C. Cardiovascular system changes (htn, tachycardia, hypertension, pulm oedema)
D. Fluid overload (+ve fluid balance; clinical improvement following diuresis)
E. Positive biomarker (e.g. BNP or NT-pro BNP) 2/2
C. Cardiovascular system changes (htn, tachycardia, hypertension, pulm oedema)
D. Fluid overload (+ve fluid balance; clinical improvement following diuresis)
E. Positive biomarker (e.g. BNP or NT-pro BNP) 2/2
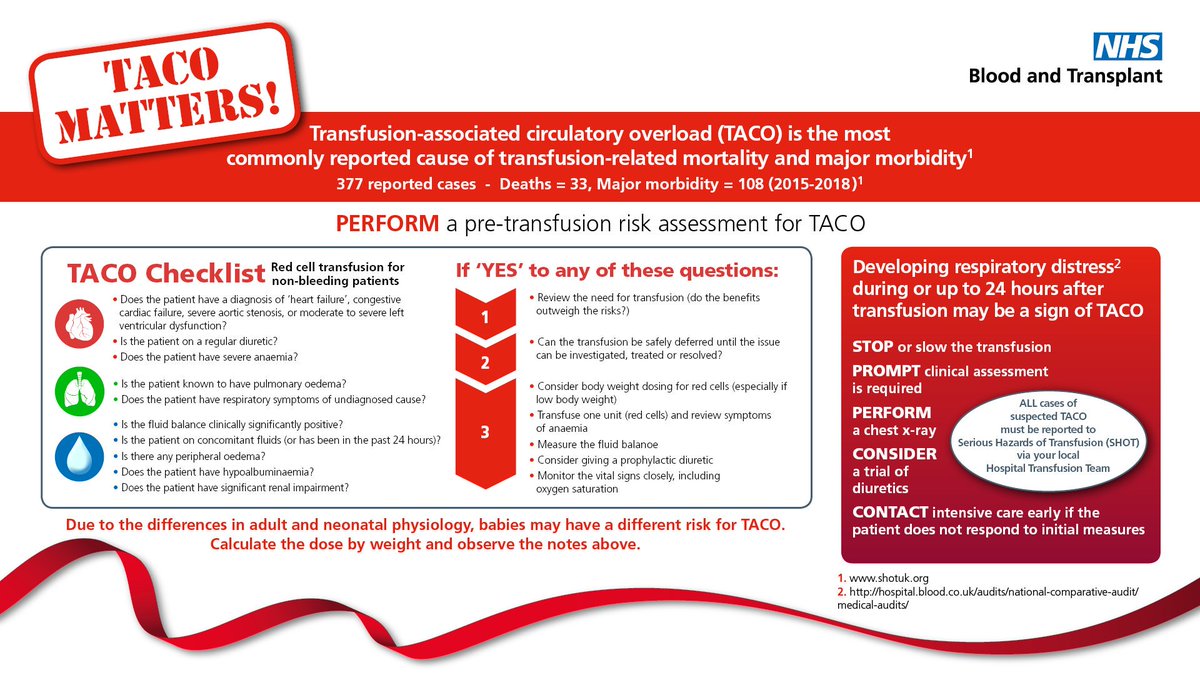
In the audit 89% of patients aged >60 had at least 1 additional risk factor for TACO. For such a common problem, there are very little data to support appropriate action to take in patients with risk factors.
Results of the NCA can be found here
hospital.blood.co.uk/audits/nationa…
Suffice to say, we could do better at assessing risk, monitoring and treating appropriately!
hospital.blood.co.uk/audits/nationa…
Suffice to say, we could do better at assessing risk, monitoring and treating appropriately!
• • •
Missing some Tweet in this thread? You can try to
force a refresh