@carlheneghan mindfully preparing for his talk on why we need a UK Sunshine Act to help solve the problem of conflicts of interest in medicine @OxEBHC @CebmOxford @EBM_Live @OxPrimaryCare
#COI #EBM
#COI #EBM

Starts with the story of Rofecoxib (Vioxx).
Presents the evidence that didn’t get into the NEJM because one of the study authors was a paid consultant on the drug company producing Vioxx.
#COI #EBM #EBMmanifesto
Presents the evidence that didn’t get into the NEJM because one of the study authors was a paid consultant on the drug company producing Vioxx.
#COI #EBM #EBMmanifesto

Carl recalls that he prescribed Vioxx and is vexed by the probability of harm he may have caused. Due to a COI impacting on the evidence he used to inform his medical practice.
And this was preventable if a better system was in place.
And this was preventable if a better system was in place.

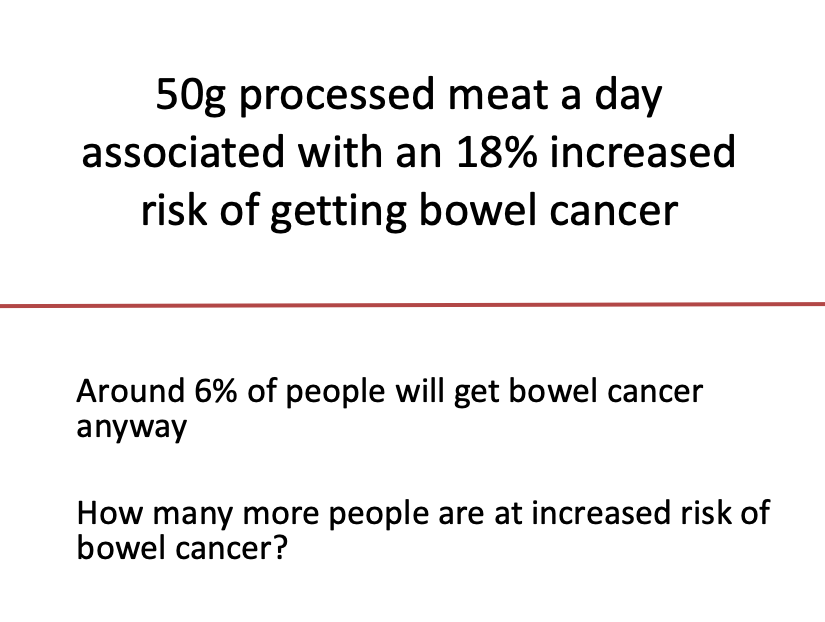
This slide is always revealing.
“Conflicts don’t impact on me. But they do on my peers”.
amjmed.com/article/S0002-…
“Conflicts don’t impact on me. But they do on my peers”.
amjmed.com/article/S0002-…

Another great paper on the impact of bias and blind spots on interpretations of evidence resulting from COI. 

The UK doesn’t have the equivalent of the Sunshine Act. What was agreed was the ABPI proposal. The key issue = it’s VOLUNTARY.
That presents problems, as @bengoldacre neatly points out.
That presents problems, as @bengoldacre neatly points out.

Voluntary systems DO NOT WORK.
Others have realised this. And acted.
Look at this list. All countries outside the US who have a Sunshine Act on DOIs. It’s revealing based on OMISSIONS not inclusions.
#COI #EBM #EBMmanifesto
Others have realised this. And acted.
Look at this list. All countries outside the US who have a Sunshine Act on DOIs. It’s revealing based on OMISSIONS not inclusions.
#COI #EBM #EBMmanifesto

Carl’s paper with @mgtmccartney in @TheLancet puts the issues forward.
And they are starting this website (will share link if I find it). Just a small matter of waiting for @GOVUK and @gmcuk to make this standard practice. #whatareyouwaitingfor
#COI #EBM #EBMmanifesto

And they are starting this website (will share link if I find it). Just a small matter of waiting for @GOVUK and @gmcuk to make this standard practice. #whatareyouwaitingfor
#COI #EBM #EBMmanifesto


• • •
Missing some Tweet in this thread? You can try to
force a refresh