1/ Let's differentiate pyogenic from amebic liver abscess in a #Tweetorial today. We will examine DDx, risk factors, microbiology, clinical features, diagnostics, and treatment. This came from my most recent morning report. #IDTwitter #LiverTwitter #MedEd 

2/ Differential diagnosis for liver abscess:
Infectious etiologies predominate. Most are pyogenic (bacterial). Amebic (Entamoeba histolytica) and hydatid cyst (Echinococcus) important. Differentiate these from HCC or liver mets. @CPSolvers what am I missing?!
Infectious etiologies predominate. Most are pyogenic (bacterial). Amebic (Entamoeba histolytica) and hydatid cyst (Echinococcus) important. Differentiate these from HCC or liver mets. @CPSolvers what am I missing?!

3/ Pathogenesis of pyogenic liver abscess (PLA):
- Biliary obstruction (GB, cancer) most commonly
- Surgical complication, trauma
- Portal vein pyemia from intra-abdominal infection (e.g. appendicitis)
- Hematogenous seeding (endocarditis)
- Cancer tx complication (RFA, TACE)


- Biliary obstruction (GB, cancer) most commonly
- Surgical complication, trauma
- Portal vein pyemia from intra-abdominal infection (e.g. appendicitis)
- Hematogenous seeding (endocarditis)
- Cancer tx complication (RFA, TACE)


4/ Risk factors for PLA:
- DM: due to impaired PMN chemotaxis/phagocytosis
- Cirrhosis
- Immunocompromise
- Associated with underlying colorectal cancer, especially in Asia with Kleb pneumo infections
- DM: due to impaired PMN chemotaxis/phagocytosis
- Cirrhosis
- Immunocompromise
- Associated with underlying colorectal cancer, especially in Asia with Kleb pneumo infections

5/ Microbiology of PLA:
- Historically, polymicrobial (GNRs + anaerobes)
- Shifting epi in the US, with strep milleri group (anginosus, constellatus, intermedius) becoming most common (@PaulSaxMD pearl)
- Staph aureus-->think endocarditis
- 50% bacteremic
https://t.co/85YCgvIXZZinsights.ovid.com/pubmed?pmid=19…

- Historically, polymicrobial (GNRs + anaerobes)
- Shifting epi in the US, with strep milleri group (anginosus, constellatus, intermedius) becoming most common (@PaulSaxMD pearl)
- Staph aureus-->think endocarditis
- 50% bacteremic
https://t.co/85YCgvIXZZinsights.ovid.com/pubmed?pmid=19…

6/ Keep in mind community-acquired hypervirulent Klebsiella pneumoniae in patients from Taiwan/SE Asia
- RF: DM
- Metastatic infections in 10-16%: meningitis, endophtathalmitis, septic emboli
- Virulence factors: K1/K2 hypercapsule, unique siderophores
https://t.co/F6HheIloHHncbi.nlm.nih.gov/pmc/articles/P…

- RF: DM
- Metastatic infections in 10-16%: meningitis, endophtathalmitis, septic emboli
- Virulence factors: K1/K2 hypercapsule, unique siderophores
https://t.co/F6HheIloHHncbi.nlm.nih.gov/pmc/articles/P…

7/ Clinical features/Diagnosis of PLA:
- Fever/Chills, RUQ Pain, N/V
- Leukocytosis, elevated CRP, elevated AST/ALT/bilirubin/ALP
- CT & US both useful for diagnosis
- Get blood cultures!
- Cultures from abscess useful for etiology


- Fever/Chills, RUQ Pain, N/V
- Leukocytosis, elevated CRP, elevated AST/ALT/bilirubin/ALP
- CT & US both useful for diagnosis
- Get blood cultures!
- Cultures from abscess useful for etiology

8/ Treatment of PLA:
- Source control essential: percutaneous catheter>surgery
- Empiric antibiotics: ceftriaxone + metronidazole usually (@UpToDate)
- Consider vanc if MRSA concerns (endocarditis)
- Duration: 4-6 weeks IV-->PO, but evidence limited



- Source control essential: percutaneous catheter>surgery
- Empiric antibiotics: ceftriaxone + metronidazole usually (@UpToDate)
- Consider vanc if MRSA concerns (endocarditis)
- Duration: 4-6 weeks IV-->PO, but evidence limited



9/ We will now focus on amebic liver abscess (ALA) from the protozoan Entamoeba histolytica!
- E. hystolytica is usually asymptomatic (90%)
- Most commonly causes dysentery, but also known for liver abscess, brain/heart/lung involvement
Image: https://t.co/PPkLddAvtunejm.org/doi/full/10.10…

- E. hystolytica is usually asymptomatic (90%)
- Most commonly causes dysentery, but also known for liver abscess, brain/heart/lung involvement
Image: https://t.co/PPkLddAvtunejm.org/doi/full/10.10…

10/ There are 4 known species of Entamoeba:
- E. histolytica
- E. dispar (non-pathogenic)
- E. moshkovskii (?pathogen)
- E. bangladeshi (?pathogen)
We will be focusing on E. histolytica, but E. dispar is an important confounder in epidemiology & diagnostics (see below)
- E. histolytica
- E. dispar (non-pathogenic)
- E. moshkovskii (?pathogen)
- E. bangladeshi (?pathogen)
We will be focusing on E. histolytica, but E. dispar is an important confounder in epidemiology & diagnostics (see below)
11/ E. histolytica exists as 2 forms:
Cysts (figure 1): survive for weeks in environment due to thick walls, transmit the disease via feces
Trophozooites (figure 2): die in environment & stomach acid, invade colonic walls (amebic dysentery) into blood stream (liver, brain, etc)


Cysts (figure 1): survive for weeks in environment due to thick walls, transmit the disease via feces
Trophozooites (figure 2): die in environment & stomach acid, invade colonic walls (amebic dysentery) into blood stream (liver, brain, etc)


12/ E. histolytica lifecycle:
- Excreted into feces via cysts which transmit disease via fecal-oral route
- Trophozooites multiply and make cysts in the colon
Images: @CDCgov


- Excreted into feces via cysts which transmit disease via fecal-oral route
- Trophozooites multiply and make cysts in the colon
Images: @CDCgov


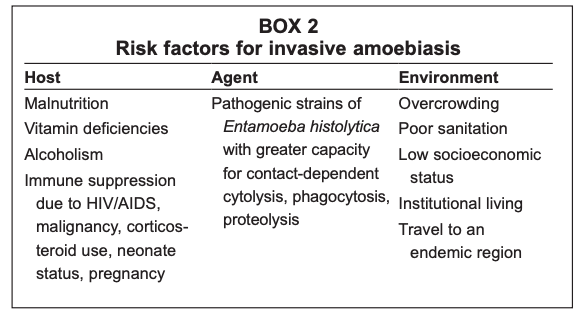
13/ Risk factors for ALA:
- Male (10:1, likely due to EtOH-induced liver damage, as colonic amebiasis 1:1)
- MSM, Institutionalization, Immunosuppression
- Endemic regions: Mexica, Central/South America, India, Africa
- 35% in short term travelers (<6w)
https://t.co/N5jBTXzx9gncbi.nlm.nih.gov/pmc/articles/P…


- Male (10:1, likely due to EtOH-induced liver damage, as colonic amebiasis 1:1)
- MSM, Institutionalization, Immunosuppression
- Endemic regions: Mexica, Central/South America, India, Africa
- 35% in short term travelers (<6w)
https://t.co/N5jBTXzx9gncbi.nlm.nih.gov/pmc/articles/P…

14/ Clinical presentation of ALA:
- Incubation period of weeks to years
- Fever, RUQ pain for ~2 weeks
- Referred pain to R shoulder/chest, epigastric, pleuritic
- Diarrhea in ~1/3rd
- Can rupture into peritoneum, pleura, or pericardium uncommonly
- Incubation period of weeks to years
- Fever, RUQ pain for ~2 weeks
- Referred pain to R shoulder/chest, epigastric, pleuritic
- Diarrhea in ~1/3rd
- Can rupture into peritoneum, pleura, or pericardium uncommonly

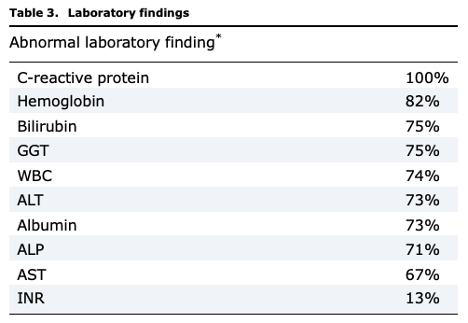
15/ Lab/Imaging findings of ALA:
- 75% leukocytosis (WITHOUT eosinophilia)
- 2/3rds elevated AST/ALT, 80% elevated ALP
- Anemia, hyperbilirubinemia, and hypoalbuminemia seen
- R hemidiaphragm elevation on CXR in 1/3rd
- CT & US useful
- 75% leukocytosis (WITHOUT eosinophilia)
- 2/3rds elevated AST/ALT, 80% elevated ALP
- Anemia, hyperbilirubinemia, and hypoalbuminemia seen
- R hemidiaphragm elevation on CXR in 1/3rd
- CT & US useful

16/ Diagnostics for ALA are tricky!
Stool/aspirate microscopy
- Insensitive (only 24% in one series)
- Non-specific: cannot distinguish between pathogenic E. histolytica & non-pathogenic E. dispar (morphologically the same!)
- Need specialized lab personnel & >3 stool samples
Stool/aspirate microscopy
- Insensitive (only 24% in one series)
- Non-specific: cannot distinguish between pathogenic E. histolytica & non-pathogenic E. dispar (morphologically the same!)
- Need specialized lab personnel & >3 stool samples

17/ Serum antibody serology is great for rule out
- Detectable after 7 days of infection in 85-95% of patients (sensitive), but negative early in infection
- Persists for years, so 10-35% of uninfected have +Ab in endemic areas, cannot distinguish old from new infection
- Detectable after 7 days of infection in 85-95% of patients (sensitive), but negative early in infection
- Persists for years, so 10-35% of uninfected have +Ab in endemic areas, cannot distinguish old from new infection
18/ Stool antigen testing is very useful
- 87% sensitive, >90% specific
- Detects Gal/GalNAc lectin, specific to E. histolytica
PCR tests being developed
Summary: serum Ab & stool Ag tests are the best methods for diagnosis. Don't order stool microscopy!
- 87% sensitive, >90% specific
- Detects Gal/GalNAc lectin, specific to E. histolytica
PCR tests being developed
Summary: serum Ab & stool Ag tests are the best methods for diagnosis. Don't order stool microscopy!
19/ Treatment for ALA differs from PLA:
- Drainage is not necessary, unless uncertainty of diagnosis, lack of clinical improvement, or high risk for rupture (>10cm)
- If drained, cultures will not help for ALA, but the color might! Remember anchovy paste!


- Drainage is not necessary, unless uncertainty of diagnosis, lack of clinical improvement, or high risk for rupture (>10cm)
- If drained, cultures will not help for ALA, but the color might! Remember anchovy paste!


20/ Antibiotics for ALA:
- Metronidazole x 7-10 days for abscess
- Then need intraluminal treatment (for cysts!) with paramomycin or iodoquinol
- Metronidazole x 7-10 days for abscess
- Then need intraluminal treatment (for cysts!) with paramomycin or iodoquinol

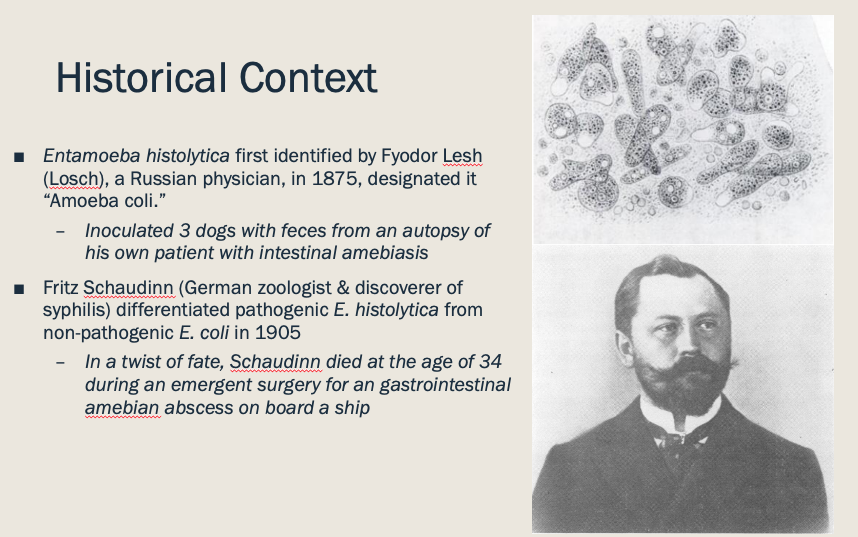
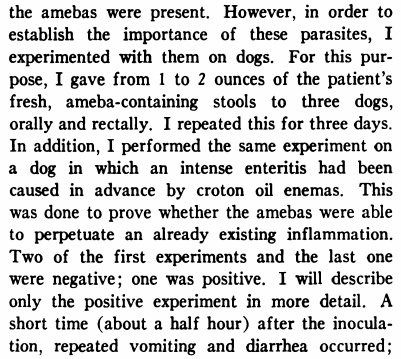
21/ Some cool history on this topic!
@AdamRodmanMD will appreciate the article about Fyodor Lesh! Science was different in the 19th century
https://t.co/3k3uxDfaeq https://t.co/SwarvnD1gancbi.nlm.nih.gov/pubmed/1098489
ncbi.nlm.nih.gov/pmc/articles/P…


@AdamRodmanMD will appreciate the article about Fyodor Lesh! Science was different in the 19th century
https://t.co/3k3uxDfaeq https://t.co/SwarvnD1gancbi.nlm.nih.gov/pubmed/1098489
ncbi.nlm.nih.gov/pmc/articles/P…
22/ That's it for this #Tweetorial. It was a long one! Appreciate feedback as always and hope you learned as much as I did on this one!
Appreciate the help on my AM report presentation from @mmcclean1 @Strongylady @MitchGoldmanMD
Appreciate the help on my AM report presentation from @mmcclean1 @Strongylady @MitchGoldmanMD

@mmcclean1 @Strongylady @MitchGoldmanMD Tagging a few who may be interested in this subject: @IUIDfellowship @IUIntMed @ebtapper @liverprof @tony_breu @thecurbsiders @UNMC_ID @DoctorJinnette @MedEdPGH @eColeID @medrants
@mmcclean1 @Strongylady @MitchGoldmanMD @IUIDfellowship @IUIntMed @ebtapper @liverprof @tony_breu @thecurbsiders @UNMC_ID @DoctorJinnette @MedEdPGH @eColeID @medrants A related post from @WuidQ in November 2019 regarding E. histolytica
https://twitter.com/WuidQ/status/1199406534855401472?s=20
@mmcclean1 @Strongylady @MitchGoldmanMD @IUIDfellowship @IUIntMed @ebtapper @liverprof @tony_breu @thecurbsiders @UNMC_ID @DoctorJinnette @MedEdPGH @eColeID @medrants @WuidQ Have found a good source for DDx as well as a radiography-based schema!
https://t.co/ULYWXmFi9Ancbi.nlm.nih.gov/pubmed/27232504

https://t.co/ULYWXmFi9Ancbi.nlm.nih.gov/pubmed/27232504

• • •
Missing some Tweet in this thread? You can try to
force a refresh















