Last week I did zoom ECG teaching.
I thought I’d use this thread to share some of the more interesting ECGs I found while prepping.
Here’s the first - May not seem remarkable at first glance but I’ve never seen it before (though I have seen something similar).
I thought I’d use this thread to share some of the more interesting ECGs I found while prepping.
Here’s the first - May not seem remarkable at first glance but I’ve never seen it before (though I have seen something similar).

Day two of #quarantinECGs.
Not as unique as yesterday but equally dramatic.
I think this ECG is a good example for a multilevel learning environment. Something immediately apparent and something more subtle for the more advanced learner.
Not as unique as yesterday but equally dramatic.
I think this ECG is a good example for a multilevel learning environment. Something immediately apparent and something more subtle for the more advanced learner.

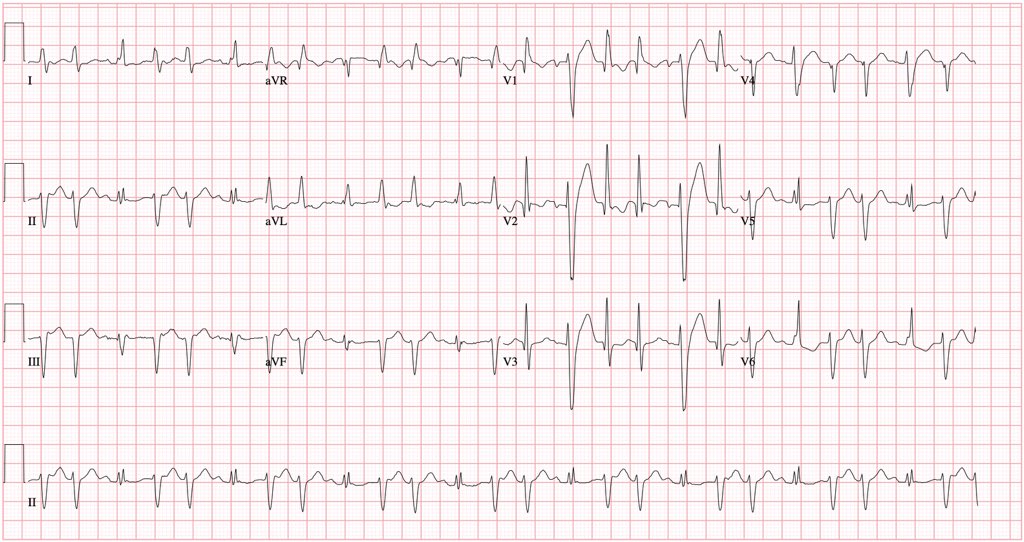
Follow-up for day 2 ECG.
This patient had been brought to hospital after having witnessed seizure in a McDonalds. Initially these were attributed to alcohol withdrawal (known use disorder). In ER was noted to have profound hypoK, hypoMg and hypoCa. Then this ECG was captured...
This patient had been brought to hospital after having witnessed seizure in a McDonalds. Initially these were attributed to alcohol withdrawal (known use disorder). In ER was noted to have profound hypoK, hypoMg and hypoCa. Then this ECG was captured...
...showing PMVT initiated by a PVC couplet. The first at a longer coupling than the second.
But, prior to PMVT there is T wave alternans. These are sudden changes in temporal heterogeneity in ventricular repolarization and are associated with impending ventricular arrhythmias.
But, prior to PMVT there is T wave alternans. These are sudden changes in temporal heterogeneity in ventricular repolarization and are associated with impending ventricular arrhythmias.

This ECG is a good example of a rate dependent LBBB.
If you look carefully the sinus rate is unchanged. There is a rate dependent LBBB when sinus conducts one to one (latter part of the ECG) but after the PVC there is a compensatory pause and the bundle recovers....
If you look carefully the sinus rate is unchanged. There is a rate dependent LBBB when sinus conducts one to one (latter part of the ECG) but after the PVC there is a compensatory pause and the bundle recovers....
...the RBBB beat is a PVC with slightly variable coupling intervals. In RBBB beats 3 and 4 the coupling is shorter and you can see the latter half of the upright P wave late in the QRS, but in beat 5 the coupling is longer and the P wave is seen early in the QRS. 

This ECG was recorded in a patient with a potassium of 8.9.
Mild ⬆️K – extracellular K results in increased conductance via Ikr ➡️ ST depression, peak T & QT shortening
Moderate ⬆️K – persistently depolarises cell membrane inactivating Na channel ➡️ wide QRS and prolonged PR..
Mild ⬆️K – extracellular K results in increased conductance via Ikr ➡️ ST depression, peak T & QT shortening
Moderate ⬆️K – persistently depolarises cell membrane inactivating Na channel ➡️ wide QRS and prolonged PR..
Severe K – sinoventricular conduction progresses to accelerated junctional with progressive QRST widening and ST-segment obliteration ➡️ smooth diphasic, sine wave.
Note – pseudo-ST segment elevation can be observed due to derangement in myocyte repolarization (same pt - K 8.1)
Note – pseudo-ST segment elevation can be observed due to derangement in myocyte repolarization (same pt - K 8.1)

#quarantinECGs day five.
Of note - some have asked for context.
Most of these ECGs are from reading outpatient tests (ie they just show up in an inbox without context - no indication, no history, no medications, etc...).
So in a lot of circumstances we are reading blind.
Of note - some have asked for context.
Most of these ECGs are from reading outpatient tests (ie they just show up in an inbox without context - no indication, no history, no medications, etc...).
So in a lot of circumstances we are reading blind.
This ECG demonstrates sinus rhythm with LBBB and PVC couplets. The PVCs are likely posterior fascicle in origin.
The point that catches some learners is the observation that the PVCs look narrower in V1 leading them to think this is PVC trigeminy.
But P waves point to SV beats
The point that catches some learners is the observation that the PVCs look narrower in V1 leading them to think this is PVC trigeminy.
But P waves point to SV beats
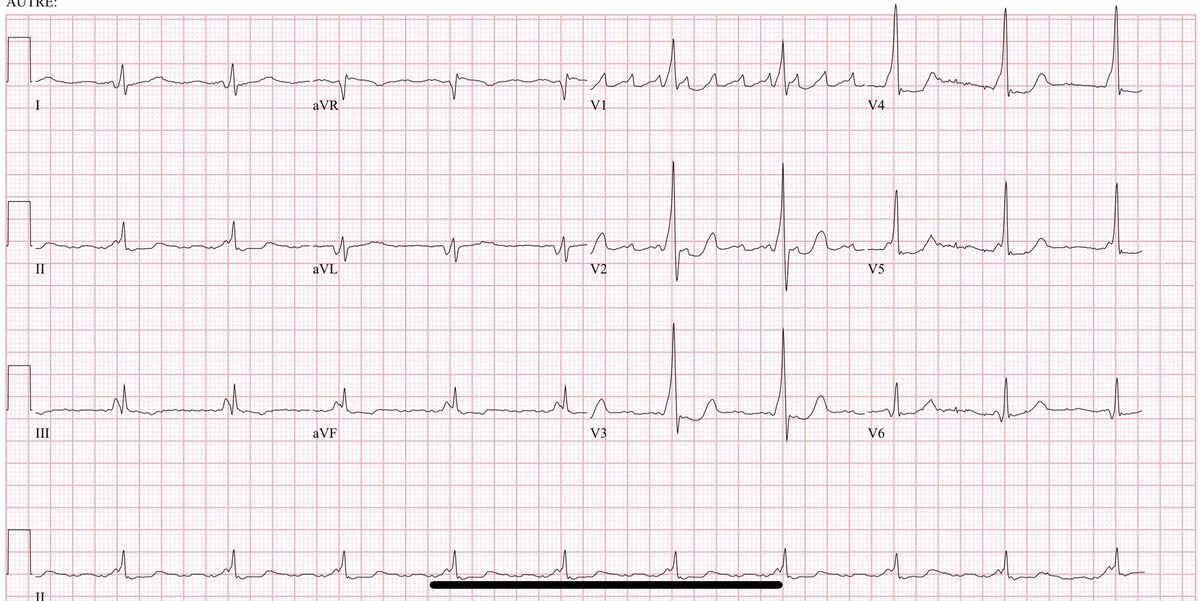
#quarantinECGs day six.
Two patients.
Same underlying medical condition.
receiving the same treatment.
Leading to the same artifact on ECG.
What is the cause of the artifact/what is the underlying condition?

Two patients.
Same underlying medical condition.
receiving the same treatment.
Leading to the same artifact on ECG.
What is the cause of the artifact/what is the underlying condition?


This ECG demonstrates the artifact observed with deep brain stimulators implanted for Parkinson’s
DBS stimulates the part of the brain involved in motor function
It’s most effective for disabling tremors, wearing-off spells & medication-induced dyskinesias, but is not a cure
DBS stimulates the part of the brain involved in motor function
It’s most effective for disabling tremors, wearing-off spells & medication-induced dyskinesias, but is not a cure
#quarantinECGs day seven.
Another ECG I’ve never seen before.
Two things are happening across this ECG.
Another ECG I’ve never seen before.
Two things are happening across this ECG.

This ECG shows SVT degenerating into self limited polymorphic VT following adenosine.
One proposed interpretation was SVT degenerating into AF with preexcitation but the SVT is likely AVNRT given the short VA interval (pseudo-S in inferior leads and pseudo-r’ in V1).
One proposed interpretation was SVT degenerating into AF with preexcitation but the SVT is likely AVNRT given the short VA interval (pseudo-S in inferior leads and pseudo-r’ in V1).
#quarantinECGs day eight. 

This ECG demonstrates complete heart block with a very slow escape rhythm. There is a clear escape in the middle of the twcibg, but right at the beginning of the ECG you see the T wave of the previous escape beat.
This ecg shows sinus rhythm with LBBB. There is a competing AIVR that is originating from the LV. This results in the 3rd and 4th beats having fusion, which narrows the QRS due to intrinsic resynchronisation (akin to what we do when we implant a CRT).
Presentation was LAD STEMI
Presentation was LAD STEMI
#quarantinECGs day ten.
What’s happening here?
And why does this electrophysiologist find it interesting?
What’s happening here?
And why does this electrophysiologist find it interesting?

This ECG shows junctional rhythm with retrograde conduction alternating between a shirt and long VA time suggesting it’s alternating between the retrograde slow and fast pathways. 

To be honest I’m not certain I can completely explain this ECG.
This is the initial post implant ECG for a @MicroPortCRMUSA Reply DR pacemaker implanted for AV block.
Breaking it down by its components. 1/n
This is the initial post implant ECG for a @MicroPortCRMUSA Reply DR pacemaker implanted for AV block.
Breaking it down by its components. 1/n
The base rate is about 65-70 bpm (the rate between two sequential paced complexes).
Some PVCs are undersensed and do not reset the timing cycle (2nd paced beat).
Others are sensed and reset the timing cycle (4th paced beat). 2/n
Some PVCs are undersensed and do not reset the timing cycle (2nd paced beat).
Others are sensed and reset the timing cycle (4th paced beat). 2/n
The AVD is super short (~80 msec) which is less than the 95 msec crosstalk interval in a Sorin device, and consistent with the “as shipped” “exercise AVD”
Interrogation 5d post implant shows stable À (1.5mV & 0.75V) and V (8.5mV & 0.75V) lead parameters. 3/n
Interrogation 5d post implant shows stable À (1.5mV & 0.75V) and V (8.5mV & 0.75V) lead parameters. 3/n
#quarantinECG day twelve.
Got delayed digging up the operative reports on the previous ECG to try and explain it...
Whats going on here?
Got delayed digging up the operative reports on the previous ECG to try and explain it...
Whats going on here?

In addition to the above ECG, each of the following four ECGs were recorded in the same person. This should help point out the mechanism. 






These ECGs demonstrate an atrial flutter (look to V1) with varying normal AV nodal conduction, fusion between AV node conduction and a AP, full AP conduction, and about conduction with LBBB.
The original ECG shows pre-excitation (fusion AVN/AP) then full AP then block in both
The original ECG shows pre-excitation (fusion AVN/AP) then full AP then block in both
This ECG demonstrates a normally functioning @Medtronic pacemaker.
The patient is paced in atrium in MVP mode with a very long AVD. Note the 4th and 9th best don’t have a QRS complex between sequential P waves. This triggers the device to pace the ventricle 80ms after the AP.
The patient is paced in atrium in MVP mode with a very long AVD. Note the 4th and 9th best don’t have a QRS complex between sequential P waves. This triggers the device to pace the ventricle 80ms after the AP.

This ECG demonstrates AF with RVR. There is LBBB with discordant ST changes *BUT* looking to the high lateral leads (I, aVL) you see concordant ST elevation (ST segment and QRS in same direction) suggesting acute STEMI as per @ElenaSgarbossa criteria.
nejm.org/doi/full/10.10…
nejm.org/doi/full/10.10…

This ECG demonstrates sinus tachycardia with complete heart block.
There is a regular ventricular escape rhythm however the cycle is perturbed by the PVCs and couplets.
There is a regular ventricular escape rhythm however the cycle is perturbed by the PVCs and couplets.
This ECG demonstrates sinus rhythm with atypical rsR’ pattern in V1 due to the presence of an epsilon wave (postexcitation in the RV) with associated right précordial TWI.
There is also a PVC which may be originating from the inferior RV.
The underlying diagnosis is ARVC.
There is also a PVC which may be originating from the inferior RV.
The underlying diagnosis is ARVC.
#quarantinECGs day seventeen.
This is a particularly challenging one due to the multiple things that are going on.
@SergioPinski @adribaran @smithECGBlog @BrooksWalsh
This is a particularly challenging one due to the multiple things that are going on.
@SergioPinski @adribaran @smithECGBlog @BrooksWalsh

This ECG is done post transplant. It shows sinus rhythm ~80 bpm in the recipients stump with sinus bradycardia in the donor heart with escape capture bigeminy.
There is also a RBBB and LAFB.
There is also a RBBB and LAFB.
This ECG shows AF with 2 QRS morphologies, which coincidentally occur at lead transitions
One is an irregular LBBB of native conduction
The other is wide and regular -> V pacing during advanced AV block.
Spikes are hard to see but the context of AF+LBBB prompts a closer look
One is an irregular LBBB of native conduction
The other is wide and regular -> V pacing during advanced AV block.
Spikes are hard to see but the context of AF+LBBB prompts a closer look
#quarantinECGs day nineteen. 

This ECG shows dextrocardia.
- Abnormal precordial R wave progression with R/S ratio >1 in V1-2 and <1 in V6
- “Global negativity" in lead I (inverted P wave, negative QRS, inverted T wave) with inverted P wave in lead II
- Right Axis Deviation
- Upright QRS complex in aVR.
- Abnormal precordial R wave progression with R/S ratio >1 in V1-2 and <1 in V6
- “Global negativity" in lead I (inverted P wave, negative QRS, inverted T wave) with inverted P wave in lead II
- Right Axis Deviation
- Upright QRS complex in aVR.

#quarantinECGs day twenty. 

This ECG demonstrates automatic atrial tachycardia. The tachycardia is interesting as it fires at two different rate (slower in the first half, faster in the second)
Middle section has termination with A (simultaneous A termination and AV block)
There are only 2 sinus beats.
Middle section has termination with A (simultaneous A termination and AV block)
There are only 2 sinus beats.
• • •
Missing some Tweet in this thread? You can try to
force a refresh

















