▶️300k+ surgeries for pelvic organ prolapse (POP) each year in US
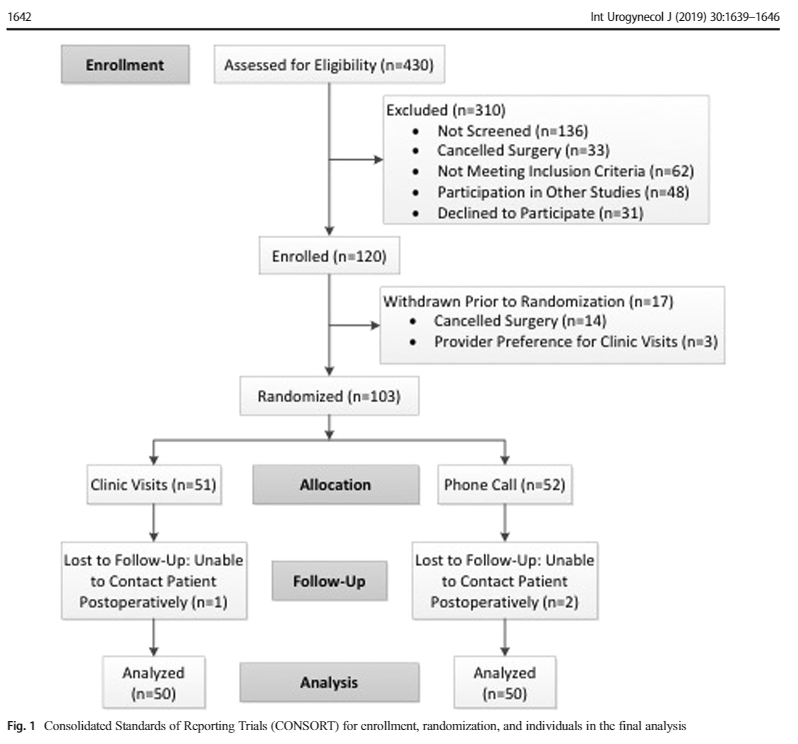
▶️Authors aimed a non-inferiority, RCT comparing routine postop outpatient clinic x telephone calls. 3/16
Exclusion criteria: pregnant or incarcerated or if the surgeon decided that F/U was needed to be in-person
4/16
Allocation:sequentially numbered, sealed, opaque 📩
🥇 outcome: pt satisfaction – S-CAHPS (Consumer Assessment of Health Providers and Systems Surgical Care Surgery) 5/16
1 – Info to prepare for surgery;
2 – Surgeon communication preop period
3 – Surgeon attentiveness on the day of surgery;
6/16
4 – Info to help during recovery
5 – Surgeon communication after surgery;
6 – Quality of office staff
7 – Overall surgeon rating
8/16
Sample size: S-CAPS scores for the global response score: 90% to represent success in both control and experimental groups, 80% power, alpha 0.025, 15% non-inferior limit: 100 pts, 50 each group.
F/U intervals (1-2,6 and 12 wks) = adverse events (AE´s) and unscheduled emergency and PC visits.
At 3 mo = final S-CAHPS, PFDI-20 and pain scales administered
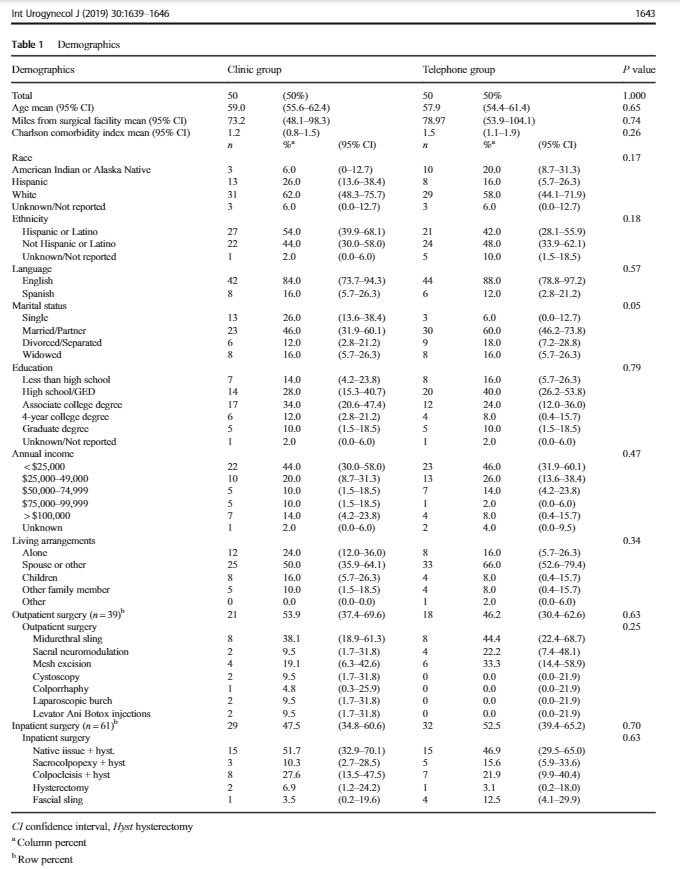
Demographics similar between groups, 48% Hispanic. Outpatient sx: MUS, sacral neuromodulation, cysto, #mesh excision, Intravesical botulinum toxin, lap Burch, colporrhaphy.In-patient sx:native tissue POP repair, sacrocolpopexy,colpocleisis,fascial sling
AE´s no # between groups. Telephone postop care did not increase frequency of emergency or PC visits. PFDI-20 scores improved in both groups with no # between them. Pain scores did not # between groups.
Limitations of the study – was not powered to evaluate other parts of postop experience, such as delayed ureteral injury. Selection bias: recruited pts lived 40+ miles far from the hospital
Strengths – novel approach to post-op care and itr thorough assessment of health care quality in the post-op setting. Reduction in outpatient visits – improving costs and decrease bureaucracy.