nature.com/articles/s4157…
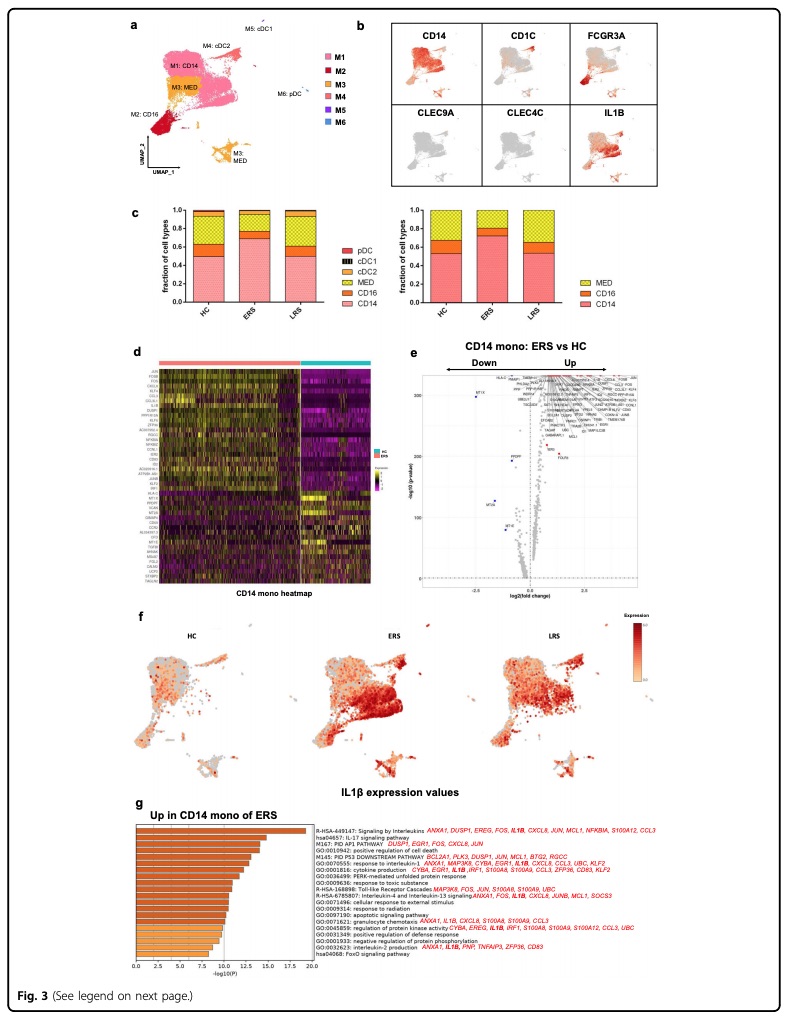
thelancet.com/journals/lanrh…
medrxiv.org/content/10.110…
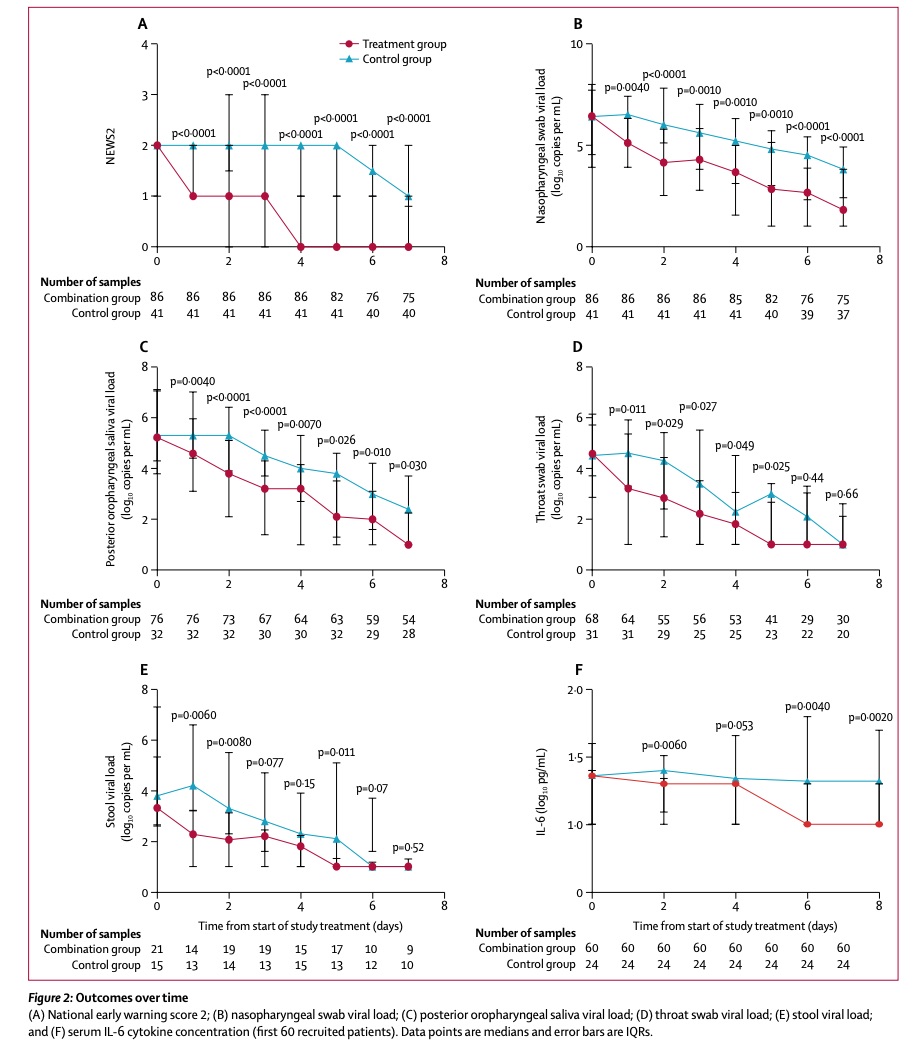
thelancet.com/journals/lance…
medrxiv.org/content/10.110…
wsj.com/articles/resea…
nature.com/articles/s4142…
onlinejacc.org/content/early/…