PROSEVA, a trial of proning in ARDS, demonstrated a 16.8% ARR
pubmed.ncbi.nlm.nih.gov/23688302/
Low tidal volumes -the most robustly reproduced effect in ARDS – had an 8.8% ARR
pubmed.ncbi.nlm.nih.gov/10793162/
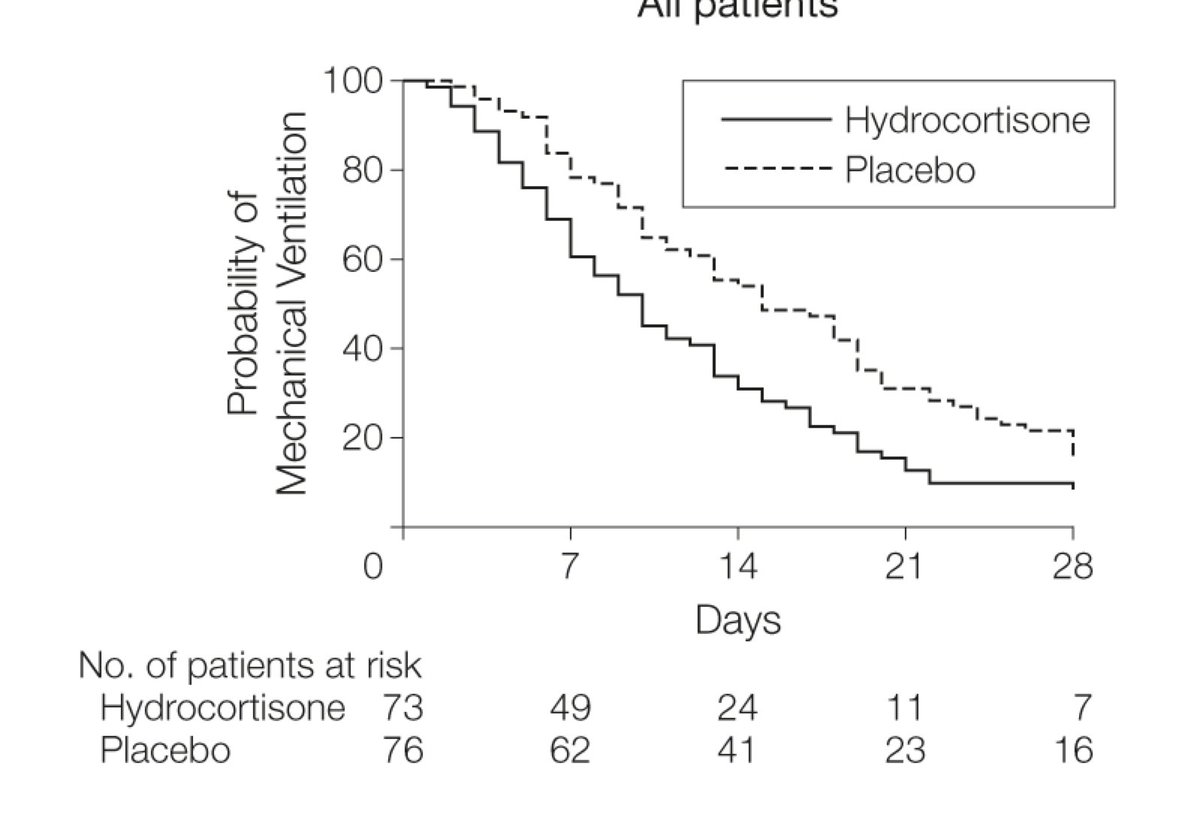
Meduri and colleagues suggested steroids reduced duration of ventilation
pubmed.ncbi.nlm.nih.gov/17426195/
pubmed.ncbi.nlm.nih.gov/16625008/
pubmed.ncbi.nlm.nih.gov/30155260/
pubmed.ncbi.nlm.nih.gov/29490185/
pubmed.ncbi.nlm.nih.gov/24232462/
pubmed.ncbi.nlm.nih.gov/17426195/
pubmed.ncbi.nlm.nih.gov/21427372/
pubmed.ncbi.nlm.nih.gov/21666444/
pubmed.ncbi.nlm.nih.gov/25289930/
pubmed.ncbi.nlm.nih.gov/7067052/
link.springer.com/chapter/10.100…
Yes -indeed have already prescribed it.