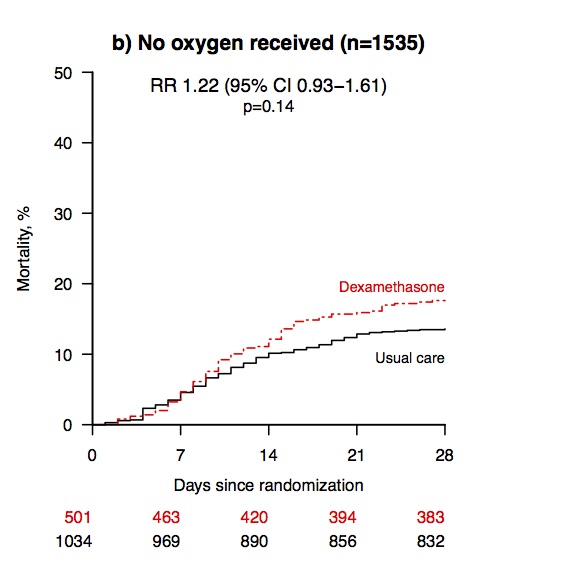
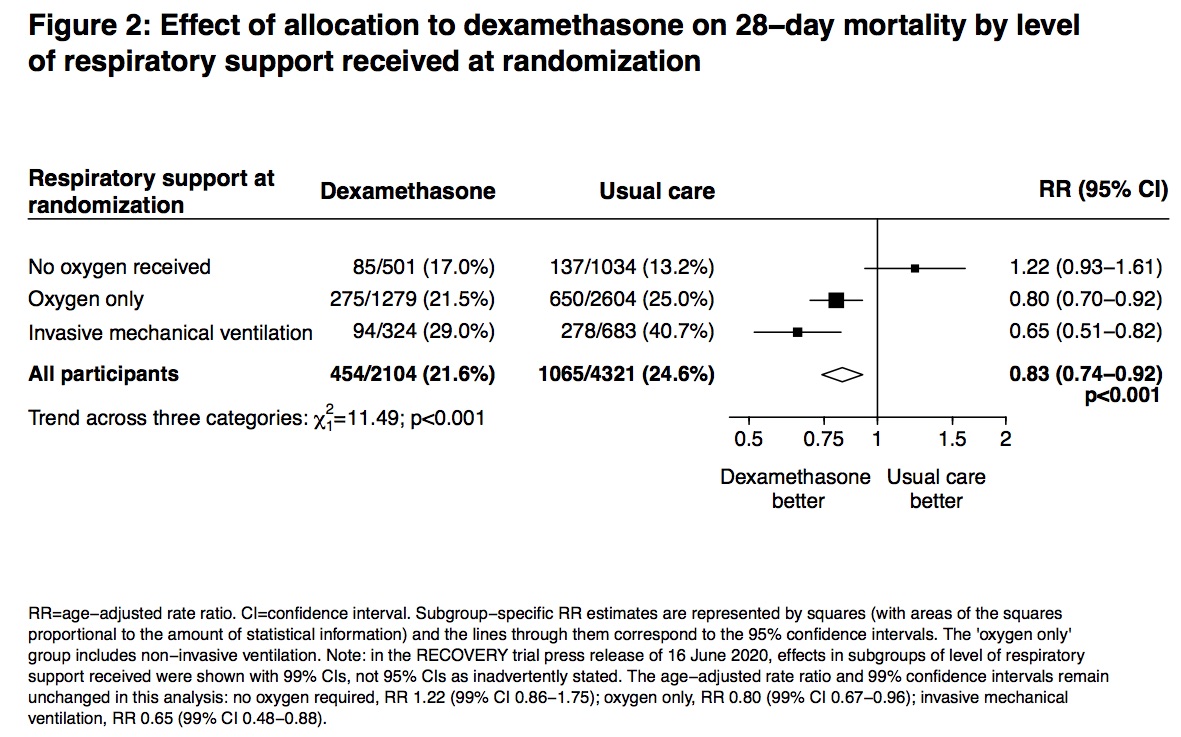
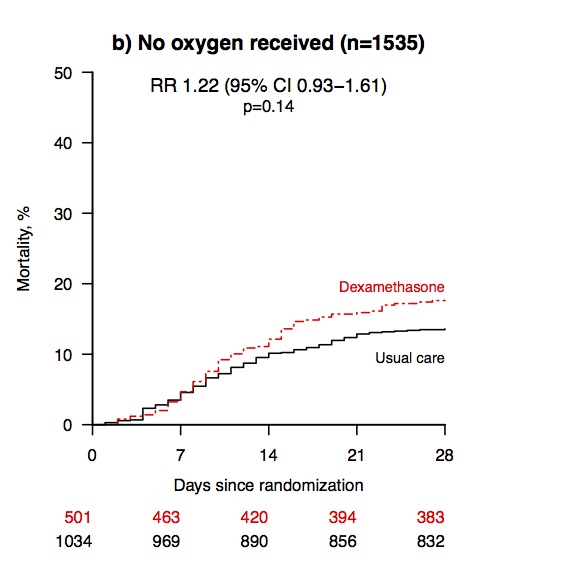
So an important issue is *which* patients should get dexamethasone and *when* in the course of their illness? 15/
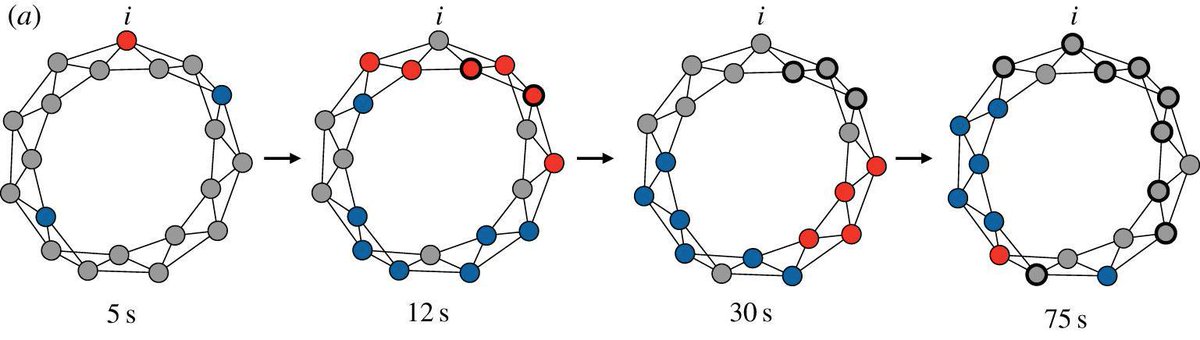
I think primary reason COVID19 CFR is declining is younger average age of people currently getting the virus (which is much deadlier in older patients than young ones – ). 29/