Time for some #SpacedRepetition: @CPSolvers
Chat recap of the #ClinicalPearls #VirtualMorningReport
June 29th Day 84: clinicalproblemsolving.com/morning-report…
w/ @RezidentMD @DxRxEdu @rabihmgeha
Case Overview by @haematognomist
Teaching points by @sukritibanthiya clinicalproblemsolving.com/wp-content/upl…
Chat recap of the #ClinicalPearls #VirtualMorningReport
June 29th Day 84: clinicalproblemsolving.com/morning-report…
w/ @RezidentMD @DxRxEdu @rabihmgeha
Case Overview by @haematognomist
Teaching points by @sukritibanthiya clinicalproblemsolving.com/wp-content/upl…
Let’s start with a problem representation:
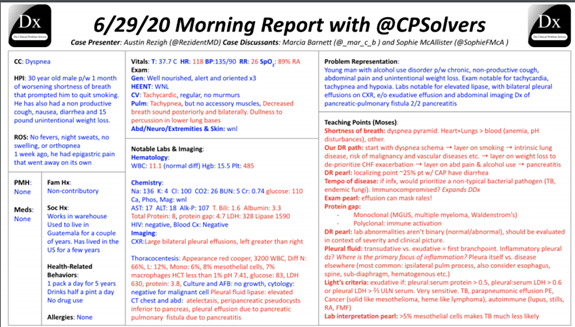
A 30 yo M from Guatemala w/ a PMH of ETOH abuse who works in a warehouse presents w/ 1month of worsening SOB, non-productive cough, nausea, diarrhea, & 15 lb weight loss was found to be tachy, hypoxic, & tachypneic w/ 🔽 BS bilaterally
A 30 yo M from Guatemala w/ a PMH of ETOH abuse who works in a warehouse presents w/ 1month of worsening SOB, non-productive cough, nausea, diarrhea, & 15 lb weight loss was found to be tachy, hypoxic, & tachypneic w/ 🔽 BS bilaterally
thinking about dyspnea pyramid right off the bat - pulmonary (airway, vasculature, parenchyma, etc.), cardiac, “bad” blood (anemia, carboxyhemoglobinemia) and acid-base disorders
Lung>blood>Heart
Tachycardia always gets our attention as does the pulse ox
Lung>blood>Heart
Tachycardia always gets our attention as does the pulse ox
weight loss is super concerning too
There is an association of smoking cessation with viral hepatitis - but that probably does not explain the dyspnea - could explain the weight loss. onlinelibrary.wiley.com/doi/abs/10.111…
There is an association of smoking cessation with viral hepatitis - but that probably does not explain the dyspnea - could explain the weight loss. onlinelibrary.wiley.com/doi/abs/10.111…

With Hep A ~50% of people lose taste for smoking
pubmed.ncbi.nlm.nih.gov/18134670/ A review from 1949!!
A mechanism for nicotine aversion ncbi.nlm.nih.gov/pmc/articles/P…
Legionaries’ disease would fit in nicely, but feel the time course does not fit as you would expect a shorter duration
pubmed.ncbi.nlm.nih.gov/18134670/ A review from 1949!!
A mechanism for nicotine aversion ncbi.nlm.nih.gov/pmc/articles/P…
Legionaries’ disease would fit in nicely, but feel the time course does not fit as you would expect a shorter duration
Other possibilities like HIV or Lymphoma. In Latin America this would be TB until proven otherwise
The indolent infection angle with that exposure
hypersensitivity pneumonitis fits his respiratory symptoms but not his GI symptoms ncbi.nlm.nih.gov/pmc/articles/P…
The indolent infection angle with that exposure
hypersensitivity pneumonitis fits his respiratory symptoms but not his GI symptoms ncbi.nlm.nih.gov/pmc/articles/P…
Pancreatitis can lead to ARDS could this explain the effusions?
Who has seen a pseudocyst causing pleural effusion? Pancreatic pseudocyst - unusual cause - but usually unilateral effusion
Bilateral effusion - still makes me think of heart disease
Who has seen a pseudocyst causing pleural effusion? Pancreatic pseudocyst - unusual cause - but usually unilateral effusion
Bilateral effusion - still makes me think of heart disease
Really interested to see if the labs take a fuNKy turn
TB screening among HIV-infected individuals recommend screening using four TB symptoms (current cough, fever, weight loss, and night sweats).
TB screening among HIV-infected individuals recommend screening using four TB symptoms (current cough, fever, weight loss, and night sweats).

How common is nightsweats? In one study night sweats were reported in 60.8% which gave specificity of 40% & a negative predictive value of 97%. ncbi.nlm.nih.gov/pmc/articles/P…
Here are some presenting sxms in TB, "However, in the early stages of disease, symptoms might be absent as shown by community-based active case finding in which about 1in4 culture-confirmed cases of pulmonary tuberculosis were reported to be asymptomatic." sciencedirect.com/science/articl…
What about his Thrombocytosis? Chronic intracellular infection vs solid malignancy

https://twitter.com/RosenelliEM/status/1278137332366000130

And his Protein Gap is……huge
Here is a refresher infographic by @AnnKumfer
As for the effusions, we need some fluid. US guided!
Here is a refresher infographic by @AnnKumfer
As for the effusions, we need some fluid. US guided!

TB pleural effusion is challenging to diagnose. TB pleural effusion would have high lymphocyte count, low or absent mesothelial cells, ADA>45
If it is an exudate - then ADA helps us distinguish between TB and cancer - the 2 most common causes of exudative pleural effusion
If it is an exudate - then ADA helps us distinguish between TB and cancer - the 2 most common causes of exudative pleural effusion
In the US the ADA is not a helpful test, there are many things that can cause a false + test, & since the prevalence of TB in the US is much lower than other dxs that cause an elevation, it is hard to interpret. As a result, hopkins removed it as an option
Thanks @TxID_Edu
Thanks @TxID_Edu
Another pearl w/ADA, it should only be sent in lymphocytic fluid. in neutrophilic predominant fluid, it will likely be a false + from the neutrophils
Lights Criteria pearls : pleural protein: serum protein > 0.5, pleural LDH: serum LDH > 0.6, pleural LDH > 2/3 ULN
Lights Criteria pearls : pleural protein: serum protein > 0.5, pleural LDH: serum LDH > 0.6, pleural LDH > 2/3 ULN

What about the copper color of his pleural fluid? Pleural Fluid: Visual Appearance and Etiology. pulmonarychronicles.com/index.php/pulm…
pH of pleural fluid is an indicator of empyema - if low < 7.2, And glucose <60 patient will need a chest tube
pH of pleural fluid is an indicator of empyema - if low < 7.2, And glucose <60 patient will need a chest tube

Criteria for having a chest tube includes complex paraneumonic effusion: ph<7.2, glucose <40, LDH>1000 or frank empyema
The presence of pus (direct diagnosis of empyema), positive Gram stain, or culture in the pleural fluid (complicated parapneumonic)
The presence of pus (direct diagnosis of empyema), positive Gram stain, or culture in the pleural fluid (complicated parapneumonic)
another pearl with ADA, it should only be sent in lymphocytic fluid. in neutrophilic predominant fluid it will likely be a false positive from the neutrophils
Lights Criteria pearls : pleural protein: serum protein > 0.5, pleural LDH: serum LDH > 0.6, pleural LDH > 2/3 ULN
Lights Criteria pearls : pleural protein: serum protein > 0.5, pleural LDH: serum LDH > 0.6, pleural LDH > 2/3 ULN

What about the copper color of his pleural fluid? Pleural Fluid: Visual Appearance and Etiology.
pulmonarychronicles.com/index.php/pulm…
pulmonarychronicles.com/index.php/pulm…

pH of pleural fluid is an indicator of empyema - if low < 7.2, And glucose <60 patient will need a chest tube
Criteria for having a chest tube includes complex paraneumonic effusion: ph<7.2, glucose <40, LDH>1000 or frank empyema
Criteria for having a chest tube includes complex paraneumonic effusion: ph<7.2, glucose <40, LDH>1000 or frank empyema
Indications for Tube Thoracotomy jtcvs.org/article/S0022-…
Impressive history of Dr Richard Light - as inspiration for all the trainees - he published his Light’s criteria as a medical resident! sciencedirect.com/science/articl…
Impressive history of Dr Richard Light - as inspiration for all the trainees - he published his Light’s criteria as a medical resident! sciencedirect.com/science/articl…
TB is unlikely if there are more than 5% mesothelial cells
And the final dx is….
Pancreaticopleural fistula. Check the pleural fluid amylase and it should be high
And the final dx is….
Pancreaticopleural fistula. Check the pleural fluid amylase and it should be high
The patient had only one well visualized fistula on ERCP though had more than one area of ductal injury he ended up getting a 14cm stent of his pancreatic duct to fix it
@RezidentMD did a nice tweetorial on the topic as well,
@RezidentMD did a nice tweetorial on the topic as well,
https://twitter.com/RezidentMD/status/1277699894321569792
A shared super random fact from Arturo is that elephants dont have a pleural space and also, dogs have both of their pleural spaces connected. journals.physiology.org/doi/full/10.11…
Overview of the complications of chronic pancreatitis uptodate.com/contents/overv…
Overview of the complications of chronic pancreatitis uptodate.com/contents/overv…
Here is a review article on the management: ncbi.nlm.nih.gov/pmc/articles/P…
It is estimated to occur in 0.4% of patients w/ pancreatitis, mostly resulting from chronic alcoholic pancreatitis
Usually presents as massive & relapsing pleural effusions, often on the L and w/high amylase
It is estimated to occur in 0.4% of patients w/ pancreatitis, mostly resulting from chronic alcoholic pancreatitis
Usually presents as massive & relapsing pleural effusions, often on the L and w/high amylase
And remember: “It’s only a bias if you’re wrong.”
Check out this great infograph by @sukritibanthiya
Check out this great infograph by @sukritibanthiya

@GurleyGuy @AndreaAnampaG @AnthonyPensa @lakh_malla @PGuptaMD @YihanYangMD @DanielCLiauw @ASanchez_PS @AbelJosephMD @BrentChamMD @AndreaAnampaG @this_is_svenka @SurajNagaraj @dminter89 @Doc_Fomin @AnnKumfer @DoubleDawgMD @Anand_88_Patel @MikeRoseMDMPH @haematognomist
@matstomato @AnandJag1 @StephVSherman @MargaretL16 @aoglasser @ETSshow @gradydoctor @MohitHarshMD @HannahRAbrams @SmithaGaneshan @jackpenner @TheRealDSrini @MattSakumoto @medrants @RachelBigley1 @k_vaishnani @MeerkatMirson @matstomato @zoyaqureshy @tony_breu @ddeng_22
@Sharminzi @ArsalanMedEd @ecvasti @JonathanRyderMD @RezidentMD @GurleyGuy @appyjumpindaze @justalisongrace @DavidTHLam @BethGay45 @BrandonKinneman @rongejman @BryanCUlrich @victorekuta @danaamara1 @NishaSunkuMD @pri_athavale @BhavyaVarma12 @sargsyanz @StephVSherman
@appyjumpindaze @noahrosenberg @JFBirnbaum @chioma_ndukweau @andressa__k @PeytonNesmith @blairgolden @BP76104 @Gurpreet2015 @mBohlega @INizamuddinMD @AlexHorneMD @EricaLCrosley @AJ_Kurtzman @miniisms @dsouzl @AaronLTroy @danielgauvin07 @AdamLongMD @d_dressler92 @Chris_Lees_
@tmodarressi @DanielleEngskow @AnneArnason @AmandaGarfinkel @mBohlega @Tapatio117 @DoctorVig @travishughes @activist_doc @franklybryan @_HarryPaul_ @Baker_C23 @FZghyer @RamlaKasoziMD @_blake_smith @LizzyHastie @AzeemRathore_ @AchantaAditya @Jcortesizaguirr @ShrutiKoti
@Azooz_Asbeutah @saipeeps @JordanSell22 @RizwanDania @Kaitlyn_Rogers9 @LawrenceWuMD @buckeye_sanjay @dmottacalderon @vikramagn @maheen_ihsan @efloyd14 @cobbnotgrey @Azooz_Asbeutah @onsarigo93 @Dayyan95 @tarheel_doctor @Anouf14 @VCU_IMRes @coyefish379 @amrmousa96 @Elizabe19893579
@Gurleen_Kaur96 @AshleyGWallace @Vandylism @RWBonner91 @abhiappukutty @PeguyTelusma @3owllearning @arturohdez_i @PaulKunnath @medrachel @sukritibanthiya @abdallah_tom @OpsBug @fernandbteich @LindseyShipley8 @OpsBug @smalltownOMS @sathya27024741 @SwainNordstrom
• • •
Missing some Tweet in this thread? You can try to
force a refresh






