Time for some #SpacedRepetition: @CPSolvers @DxRxEdu, @rabihmgeha
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 2nd Day 86: clinicalproblemsolving.com/morning-report…
w/ @ABRezMed @hraza222 & Dr. Silinsky Krupnikov @Sharminzi @ArsalanMedEd
Case Overview by @AndreaAnampaG
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 2nd Day 86: clinicalproblemsolving.com/morning-report…
w/ @ABRezMed @hraza222 & Dr. Silinsky Krupnikov @Sharminzi @ArsalanMedEd
Case Overview by @AndreaAnampaG

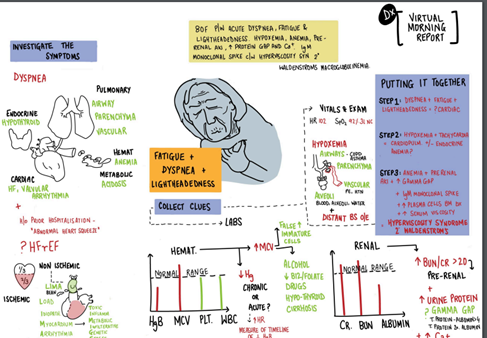
Let’s start with a problem representation:
An 80 yo F presents with worsening fatigue x 1 month, 1 week of DOE, and “dizziness” was found to be anemic, hypercalcemic with an AKI, elevated Gamma Gap with a IgM monoclonal Spike, & increased serum viscosity
An 80 yo F presents with worsening fatigue x 1 month, 1 week of DOE, and “dizziness” was found to be anemic, hypercalcemic with an AKI, elevated Gamma Gap with a IgM monoclonal Spike, & increased serum viscosity
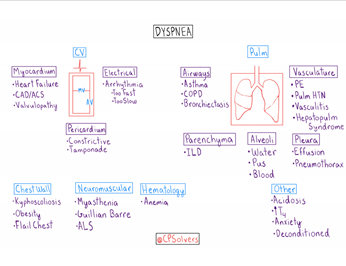
Our main focus initially is her Chief Concern:
Lightheadedness and fatigue with SOB on exertion:
Causes include: cardiac/pulmonary/anemia/metabolic
Trigger DOE schema
Lightheadedness and fatigue with SOB on exertion:
Causes include: cardiac/pulmonary/anemia/metabolic
Trigger DOE schema
She is likely not experiencing vertigo causing “dizziness” and she is likely “lightheaded” or presyncope given other complaints.
lightheadedness could mean there is intravascular depletion-near shock
we want to know about LE edema and orthopnea
lightheadedness could mean there is intravascular depletion-near shock
we want to know about LE edema and orthopnea
A significant valvulopathy can cause this too as well as constrictive pericarditis
POCUS of the heart and lungs is very helpful
POCUS calculation of EF ()
A great Podcast episode on POCUS with @medrants, acpjournals.org/doi/10.7326/A1…
POCUS of the heart and lungs is very helpful
POCUS calculation of EF ()
A great Podcast episode on POCUS with @medrants, acpjournals.org/doi/10.7326/A1…
Orthostatics and physical examination will be helpful
This dyspnea is more cardiac/anemia related because there is dizziness and possible presyncope
I also think of drug causes as well although I doubt an 80yo female is on dapsone.
This dyspnea is more cardiac/anemia related because there is dizziness and possible presyncope
I also think of drug causes as well although I doubt an 80yo female is on dapsone.
A complete drug review thinking of anticoagulant, methotrexate, nitrofurantoin, and amio. A standing BP will also be helpful.
marijuana gummies at 80. Hmmm
Heart in hypothyroidism : SVR-Increased CO-Decreased SBP low DBP Increased HR Low/normal
marijuana gummies at 80. Hmmm
Heart in hypothyroidism : SVR-Increased CO-Decreased SBP low DBP Increased HR Low/normal
Seems like a HF presentation, with the age I feel the Ddx would include: Amyloid, ICMP, Aortic stenosis, arrhythmias
Smoker and OSA— 6metre walk test may be helpful to assess pulmonary vasculature functionally
Smoker and OSA— 6metre walk test may be helpful to assess pulmonary vasculature functionally
This could be an acute presentation of a chronic condition- say anemia. but, at this juncture, w/ prev medical history, I’d worry about valvular pathology!
And now the PE:
distant BS. is the problem the lungs?
(92% on 3L) hypoxemia w/ nml auscultation -- pulm vasculature
And now the PE:
distant BS. is the problem the lungs?
(92% on 3L) hypoxemia w/ nml auscultation -- pulm vasculature
BP 142/86: Pulse pressure indicates pretty good cardiac output
CXR - we are not very good at pulmonary auscultation
when i think of distant breath sounds, i think of a shield between stetho and alveoli
CXR - we are not very good at pulmonary auscultation
when i think of distant breath sounds, i think of a shield between stetho and alveoli
tachycardia, hypoxemia, and normal lung sounds make me think of pulmonary vascular disease whether PE or pHTN
I think moderate risk Well’s - @AnnKumfer brought up PE - at least a D-dimer
MCV is high. b12 or folate def or current alcohol abuse
I think moderate risk Well’s - @AnnKumfer brought up PE - at least a D-dimer
MCV is high. b12 or folate def or current alcohol abuse
macrocytic can translate reticulocytosis: hemorrhage or hemolysis
Mild hypercalcemia an 10.7: overdosed on levothyroxine?
U/a consistent with volume contraction (SG 1.021)- so Hgb is probably lower
+protein gap, anemia, renal dysfunction
Mild hypercalcemia an 10.7: overdosed on levothyroxine?
U/a consistent with volume contraction (SG 1.021)- so Hgb is probably lower
+protein gap, anemia, renal dysfunction
Back to our favorite gamma gap: ?MM other plasma cell dyscrasias
anemia, protein gap, elevated Cr, hypercalcemia.
We certainly have to consider/evaluate for MM and granulomatous conditions.
Check SPEP, UPEP, FLC
anemia, protein gap, elevated Cr, hypercalcemia.
We certainly have to consider/evaluate for MM and granulomatous conditions.
Check SPEP, UPEP, FLC
What about her hypoxemia: Her OSA and “emphysema” probably explains hypoxemia
Is hyperviscosity a consideration? ncbi.nlm.nih.gov/books/NBK51896…
Not really kidney injury perhaps - volume contraction from diuretics - but could also have kidney injury from MM
Is hyperviscosity a consideration? ncbi.nlm.nih.gov/books/NBK51896…
Not really kidney injury perhaps - volume contraction from diuretics - but could also have kidney injury from MM
Amyloidosis should cause diastolic dysfunction
Bili and AST and LDH being normal makes intra-vascular hemolysis very unlikely.
However extravascular hemolysis can still be in the differential.
High MCV, low B12 is an example. Unlikely in this patient to be the explanation
Bili and AST and LDH being normal makes intra-vascular hemolysis very unlikely.
However extravascular hemolysis can still be in the differential.
High MCV, low B12 is an example. Unlikely in this patient to be the explanation
MCV might be indicative of increasing reticulocytosis
if going down MM path, still like hyperviscosity to link dizziness & dyspnea
Also with that anemia, wouldnt rely heavily on HbA1c for estimate of hyperglycemia that I would expect w/ someone with normal Hb & renal function
if going down MM path, still like hyperviscosity to link dizziness & dyspnea
Also with that anemia, wouldnt rely heavily on HbA1c for estimate of hyperglycemia that I would expect w/ someone with normal Hb & renal function
If she is volume contracted then her Hgb might actually be around 5 - could explain a great deal
Her FLC is high, +elevated ratio, and Kappa chains are high
This is Waldenstrom for sure
With Waldenstrom's, more likely to get hyperviscosity because IgM is a pentamer
Her FLC is high, +elevated ratio, and Kappa chains are high
This is Waldenstrom for sure
With Waldenstrom's, more likely to get hyperviscosity because IgM is a pentamer
Hypoxia probably due to hyperviscosity
hyper viscosity test not always reliable either
(CRAB symptoms: hypercalcemia, renal insufficiency, anemia and, bone lesions)
I am convinced the Rezigh twins are an endless source of great cases.
hyper viscosity test not always reliable either
(CRAB symptoms: hypercalcemia, renal insufficiency, anemia and, bone lesions)
I am convinced the Rezigh twins are an endless source of great cases.
A review on Waldenström’s Macroglobulinemia, ncbi.nlm.nih.gov/pmc/articles/P…
Monoclonal gammopathy, which is often an incidental finding, is found in 3.2–3.5% of individuals aged over 50 years.
Monoclonal gammopathy, which is often an incidental finding, is found in 3.2–3.5% of individuals aged over 50 years.
The majority of individuals (70%) develop IgG monoclonal gammopathies, followed by IgM gammopathies (10–20%). IgA gammopathies (10–17%) and biclonal (the presence of more than one monoclonal immunoglobulin) gammopathies (3–5%) are rarer
The most frequent differential diagnosis in the presence of a monoclonal IgM paraprotein is monoclonal gammopathy of undetermined significance (MGUS). statpearls.com/kb/viewarticle…
IgM MGUS is defined by an IgM serum protein of <3 g/dL, < 10% clonal lymphoplasmacytic cells in bone
IgM MGUS is defined by an IgM serum protein of <3 g/dL, < 10% clonal lymphoplasmacytic cells in bone
...marrow, and the absence of symptoms typical of WM
The risk of MGUS progressing to a malignant lymphoproliferative or related disease is 10% within the first 5 years following diagnosis
Teaching points by @sukritibanthiya: clinicalproblemsolving.com/wp-content/upl…
The risk of MGUS progressing to a malignant lymphoproliferative or related disease is 10% within the first 5 years following diagnosis
Teaching points by @sukritibanthiya: clinicalproblemsolving.com/wp-content/upl…
@GurleyGuy @AndreaAnampaG @AnthonyPensa @lakh_malla @PGuptaMD @YihanYangMD @DanielCLiauw @ASanchez_PS @AbelJosephMD @BrentChamMD @this_is_svenka @SurajNagaraj @dminter89 @Doc_Fomin @AnnKumfer @DoubleDawgMD @Anand_88_Patel @MikeRoseMDMPH @haematognomist
@matstomato @AnandJag1 @StephVSherman @MargaretL16 @aoglasser @ETSshow @gradydoctor @MohitHarshMD @HannahRAbrams @SmithaGaneshan @jackpenner @TheRealDSrini @MattSakumoto @medrants @RachelBigley1 @k_vaishnani @MeerkatMirson @matstomato @zoyaqureshy @tony_breu @ddeng_22
@Sharminzi @ArsalanMedEd @ecvasti @JonathanRyderMD @RezidentMD @GurleyGuy @appyjumpindaze @justalisongrace @DavidTHLam @BethGay45 @BrandonKinneman @rongejman @BryanCUlrich @victorekuta @DanaAmara1 @NishaSunkuMD @pri_athavale @BhavyaVarma12 @sargsyanz @StephVSherman
@appyjumpindaze @noahrosenberg @JFBirnbaum @chioma_ndukweau @andressa__k @PeytonNesmith @blairgolden @BP76104 @Gurpreet2015 @mBohlega @INizamuddinMD @AlexHorneMD @EricaLCrosley @AJ_Kurtzman @miniisms @dsouzl @AaronLTroy @danielgauvin07 @AdamLongMD @d_dressler92 @Chris_Lees_
@tmodarressi @DanielleEngskow @AnneArnason @AmandaGarfinkel @mBohlega @Tapatio117 @DoctorVig @travishughes @activist_doc @franklybryan @_HarryPaul_ @Baker_C23 @FZghyer @RamlaKasoziMD @_blake_smith @LizzyHastie @AzeemRathore_ @AchantaAditya @Jcortesizaguirr @ShrutiKoti
@Azooz_Asbeutah @saipeeps @JordanSell22 @RizwanDania @Kaitlyn_Rogers9 @LawrenceWuMD @buckeye_sanjay @dmottacalderon @vikramagn @maheen_ihsan @efloyd14 @cobbnotgrey @Azooz_Asbeutah @onsarigo93 @Dayyan95 @tarheel_doctor @Anouf14 @VCU_IMRes @coyefish379 @amrmousa96 @Elizabe19893579
@Gurleen_Kaur96 @AshleyGWallace @Vandylism @RWBonner91 @abhiappukutty @PeguyTelusma @3owllearning @arturohdez_i @PaulKunnath @medrachel @sukritibanthiya @abdallah_tom @OpsBug @fernandbteich @LindseyShipley8 @OpsBug @smalltownOMS @sathya27024741 @SwainNordstrom
• • •
Missing some Tweet in this thread? You can try to
force a refresh






