medrxiv.org/content/10.110… #safereturntowork




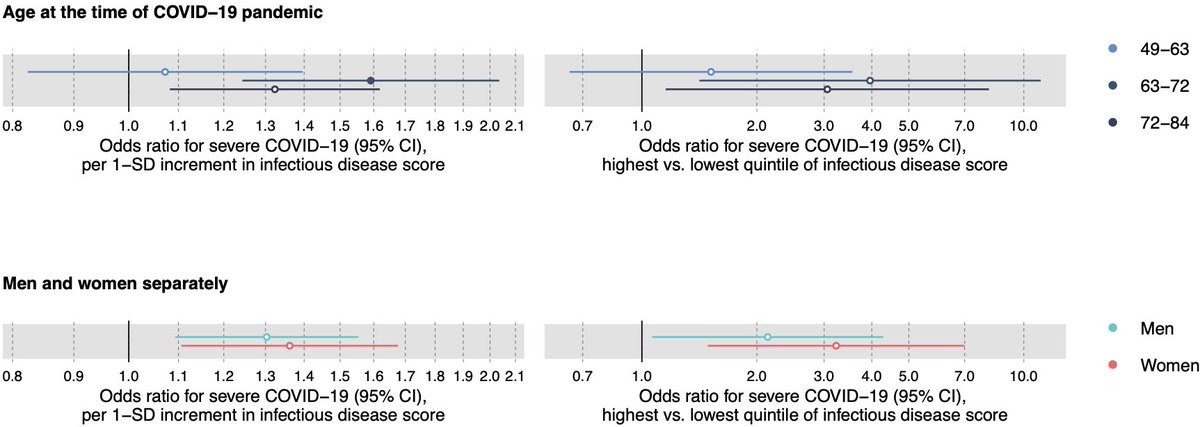
Similar strong biomarker scores can be derived for numerous chronic diseases, and apparently even infectious diseases.
nightingalehealth.com/news/nightinga…