Time for some #SpacedRepetition: @CPSolvers @DxRxEdu @rabihmgeha
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 30th Episode 104: clinicalproblemsolving.com/morning-report…
W / @Sharminzi @ArsalanMedEd @medrachel @Flower_freeland @amrmousa96
Chat recap of the #ClinicalPearls #VirtualMorningReport
July 30th Episode 104: clinicalproblemsolving.com/morning-report…
W / @Sharminzi @ArsalanMedEd @medrachel @Flower_freeland @amrmousa96
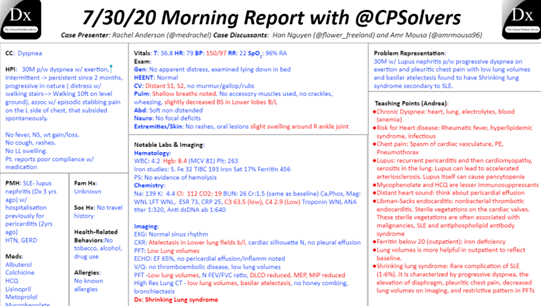
Let’s start with an initial problem representation:
A 30 y/o M w/ a PMH of lupus, pericarditis, HTN presents with 2 mon of dyspnea on exertion, worse w/ exertion, episodic CP while denying fevers, drenching night sweats, cough or weight loss
A 30 y/o M w/ a PMH of lupus, pericarditis, HTN presents with 2 mon of dyspnea on exertion, worse w/ exertion, episodic CP while denying fevers, drenching night sweats, cough or weight loss
Given her history of lupus, Autoimmune is again, as always, on the differential
He seems too young for CHF, but heart and lungs should be the initial focal point followed by anemia which is also unusual for a male at 30
He seems too young for CHF, but heart and lungs should be the initial focal point followed by anemia which is also unusual for a male at 30
This past medical history of Lupus really changes the ddx,
Given this finding, the base rate of disease (or possible causes) changes dramatically.
Would worry about pneumonitis and pleuritis as mentioned, anemia as a sequalae of lupus (autoimmune vs AOCI), or infection
Given this finding, the base rate of disease (or possible causes) changes dramatically.
Would worry about pneumonitis and pleuritis as mentioned, anemia as a sequalae of lupus (autoimmune vs AOCI), or infection
Renal etiology leading to volume overload (Lupus nephritis)
also think of exudative pleural effusion, for cardiac non bacterial endocarditis, muranitc endocarditis, pericarditis, myocarditis
We must keep non-SLE related causes alive and avoid premature closure
also think of exudative pleural effusion, for cardiac non bacterial endocarditis, muranitc endocarditis, pericarditis, myocarditis
We must keep non-SLE related causes alive and avoid premature closure
ILD can also be present in lupus as well as Lupus assoc AIHA, could cause the dyspnea
What about Libmann sacks endocarditis? ncbi.nlm.nih.gov/books/NBK53286…
It is thought to be an endothelial injury in the setting of a hypercoagulable state & most commonly affects mitral & aortic valve
What about Libmann sacks endocarditis? ncbi.nlm.nih.gov/books/NBK53286…
It is thought to be an endothelial injury in the setting of a hypercoagulable state & most commonly affects mitral & aortic valve
Physical Exam and CXR will help us narrow the differential
Would also start with a CBC, BMP, chest xray, urinalysis (looking for blood or protein), ECG, troponin, and BNP
Would also start with a CBC, BMP, chest xray, urinalysis (looking for blood or protein), ECG, troponin, and BNP
Add Physical exam of HTN of 150s/90s along with no pedal edema, but there were distant heart and breath sounds
The distant heart sounds suggests pleural or pericardial effusion
knowing his body habitus would be helpful as well as that could contribute to distant heart sounds
The distant heart sounds suggests pleural or pericardial effusion
knowing his body habitus would be helpful as well as that could contribute to distant heart sounds
The Absence of murmurs lowers, but might not fully exclude endocardial involvement
A pearl that @rabihmgeha mentioned in a previous VMR was that marantic (Libman Sacks) endocarditis more likely to present with emboli rather than valvular regurgitation
A pearl that @rabihmgeha mentioned in a previous VMR was that marantic (Libman Sacks) endocarditis more likely to present with emboli rather than valvular regurgitation
His normal SpO2 suggests dyspnea without substantial hypoxemia - we can activate that script
Now for some labs:
Nml plts and WBC along with benign BMP (nml renal function) and HCO3 of 19
But a hgb of 8.4 hmmmm (need a schema for anemia?)
Now for some labs:
Nml plts and WBC along with benign BMP (nml renal function) and HCO3 of 19
But a hgb of 8.4 hmmmm (need a schema for anemia?)

Add iron studies showing TIBC 193, iron sat 17%, ferritin 456, and S. Fe 32. (Probably iron restricted hematopoiesis)
Would like an LDH, haptoglobin to exclude AIHA
along w/ ABG as the dyspnea could be secondary to metabolic acidosis Or compensation for a respiratory alkalosis
Would like an LDH, haptoglobin to exclude AIHA
along w/ ABG as the dyspnea could be secondary to metabolic acidosis Or compensation for a respiratory alkalosis
His Anti DsDNA was repeated and is elevated at 1:160. It was repeated as it can be used to monitor SLE progress bc it usually varies with disease activity, high titers indicating active disease, low titers quiescent disease. ncbi.nlm.nih.gov/pmc/articles/P…
Did you know that Anti-(ds)DNA ab have been some of the classic diagnostic & nosological criteria of SLE since 1982
In 2012, the high titer of anti-dsDNA ab in serum accompanied by biopsy-proven lupus nephritis (LN) was accepted as an independent classification criterion for SLE
In 2012, the high titer of anti-dsDNA ab in serum accompanied by biopsy-proven lupus nephritis (LN) was accepted as an independent classification criterion for SLE
Now for some imaging:
CXR shows low lung volumes, is this bc o movement of diaphragms? Nerve or muscle complication of SLE?
PFTs show nml FEV1/FVC ratio, DLCO reduced along with reduced MEP and MIP
CXR shows low lung volumes, is this bc o movement of diaphragms? Nerve or muscle complication of SLE?
PFTs show nml FEV1/FVC ratio, DLCO reduced along with reduced MEP and MIP
The minimal changes in physical exam, shallow breathing, high RR and reduced lung volume makes us think of one thing (of course someone in the chat knew this)
Wink Wink @andressa__k
Wink Wink @andressa__k
The final dx is....
"Shrinking lung syndrome (SLS) is a rare pulmonary complication of systemic lupus erythematosus (SLE).
cureus.com/articles/32163…
"Shrinking lung syndrome (SLS) is a rare pulmonary complication of systemic lupus erythematosus (SLE).
cureus.com/articles/32163…
It is characterized by progressive dyspnea, elevation of diaphragm, pleuritic chest pain, decreased lung volumes on imaging, and restrictive pattern seen in the pulmonary function tests (PFTs)"
"Its pathophysiology remains largely unclear; however...
"Its pathophysiology remains largely unclear; however...
Hypotheses have been suggested ranging from microatelectatic changes due to lack of surfactant and increased surface tension, diaphragm fibrosis, and phrenic nerve palsy"
@GurleyGuy @AndreaAnampaG @AnthonyPensa @lakh_malla @PGuptaMD @YihanYangMD @DanielCLiauw @ASanchez_PS
@GurleyGuy @AndreaAnampaG @AnthonyPensa @lakh_malla @PGuptaMD @YihanYangMD @DanielCLiauw @ASanchez_PS
@AbelJosephMD @BrentChamMD @this_is_svenka @SurajNagaraj @dminter89 @Doc_Fomin @AnnKumfer @DoubleDawgMD @Anand_88_Patel @MikeRoseMDMPH @haematognomist @Sharminzi @ArsalanMedEd @ecvasti @JonathanRyderMD @RezidentMD @GurleyGuy @appyjumpindaze @justalisongrace @DavidTHLam
@BethGay45 @BrandonKinneman @rongejman @BryanCUlrich @victorekuta @DanaAmara1 @NishaSunkuMD @pri_athavale @BhavyaVarma12 @sargsyanz @StephVSherman @noahrosenberg @JFBirnbaum @chioma_ndukweau @andressa__k @PeytonNesmith @blairgolden @BP76104 @Gurpreet2015 @mBohlega @INizamuddinMD
@AlexHorneMD @EricaLCrosley @AJ_Kurtzman @miniisms @dsouzl @AaronLTroy @danielgauvin07 @AdamLongMD @d_dressler92 @Chris_Lees_ @tmodarressi @DanielleEngskow @AnneArnason @AmandaGarfinkel @mBohlega @Tapatio117 @DoctorVig @travishughes @activist_doc @franklybryan @_HarryPaul_
@Baker_C23 @FZghyer @RamlaKasoziMD @_blake_smith @LizzyHastie @AzeemRathore_ @AchantaAditya @Jcortesizaguirr @ShrutiKoti @Azooz_Asbeutah @saipeeps @JordanSell22 @RizwanDania @Kaitlyn_Rogers9 @LawrenceWuMD @buckeye_sanjay @dmottacalderon @vikramagn @maheen_ihsan @efloyd14
@cobbnotgrey @Azooz_Asbeutah @onsarigo93 @Dayyan95 @tarheel_doctor @Anouf14 @VCU_IMRes @coyefish379 @amrmousa96 @Elizabe19893579 @Gurleen_Kaur96 @AshleyGWallace @Vandylism @RWBonner91 @abhiappukutty @PeguyTelusma @3owllearning @arturohdez_i @PaulKunnath @medrachel
@sukritibanthiya @abdallah_tom @OpsBug @fernandbteich @LindseyShipley8 @OpsBug @smalltownOMS @sathya27024741 @SwainNordstrom @INizamuddinMD @tonlajr @RobWeberMDPhD @ABRezMed @hraza222 @Rafameed @settinger_ @TheRealDSrini
• • •
Missing some Tweet in this thread? You can try to
force a refresh






