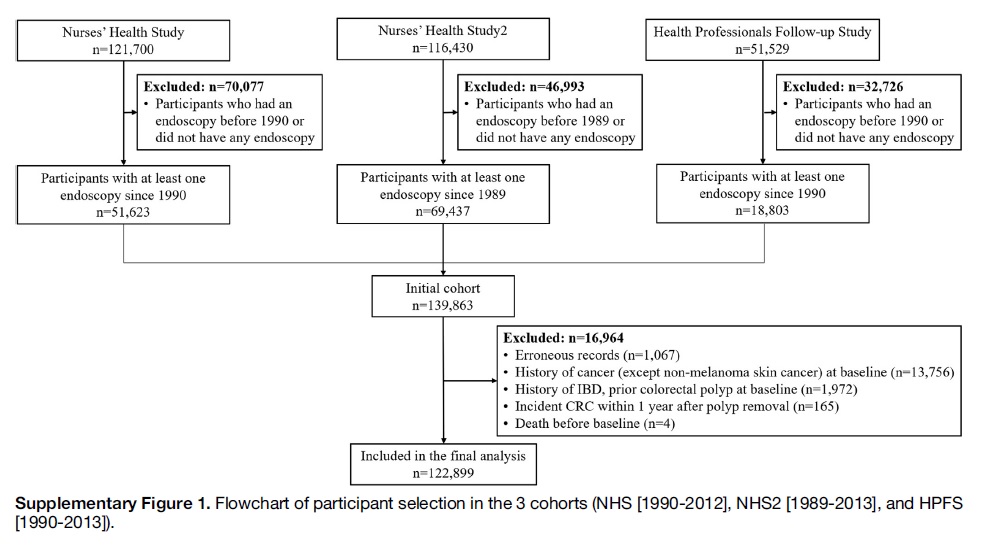
Excluded; h/o CRC in last 1yr, prior polyp, IBD, previous endoscopy #GIJC
The cox-proportional hazard regression model used to cal. HRs for CRC incidence. #GIJC
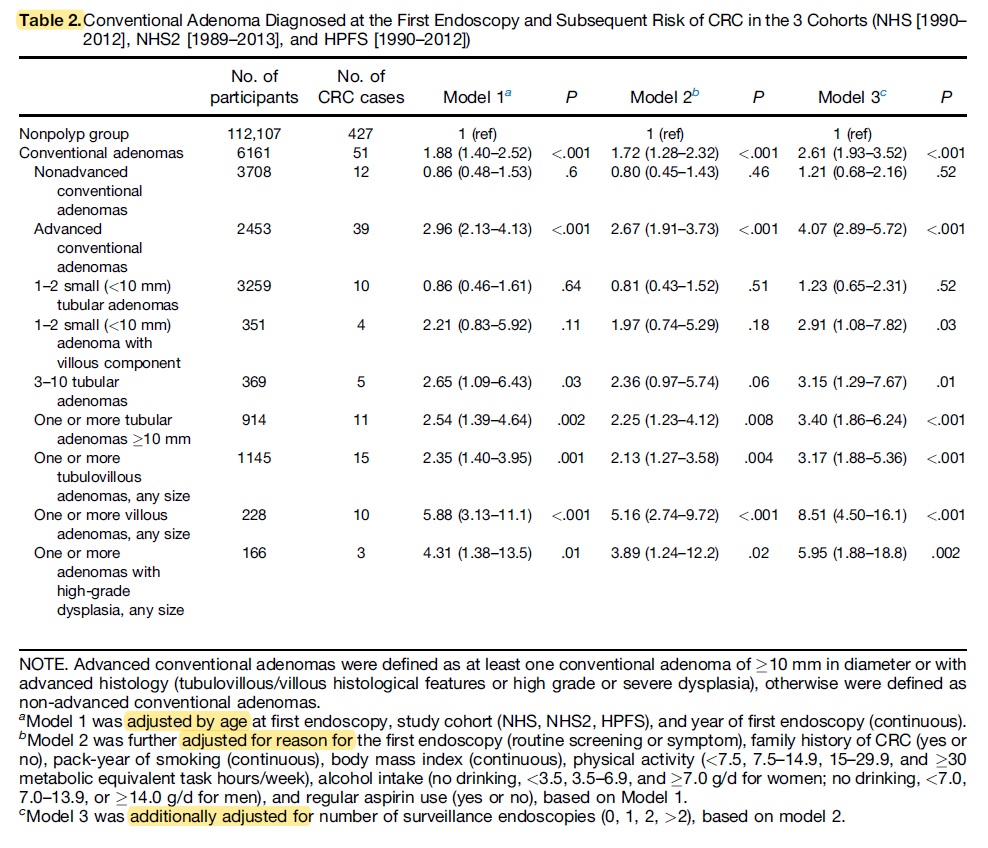
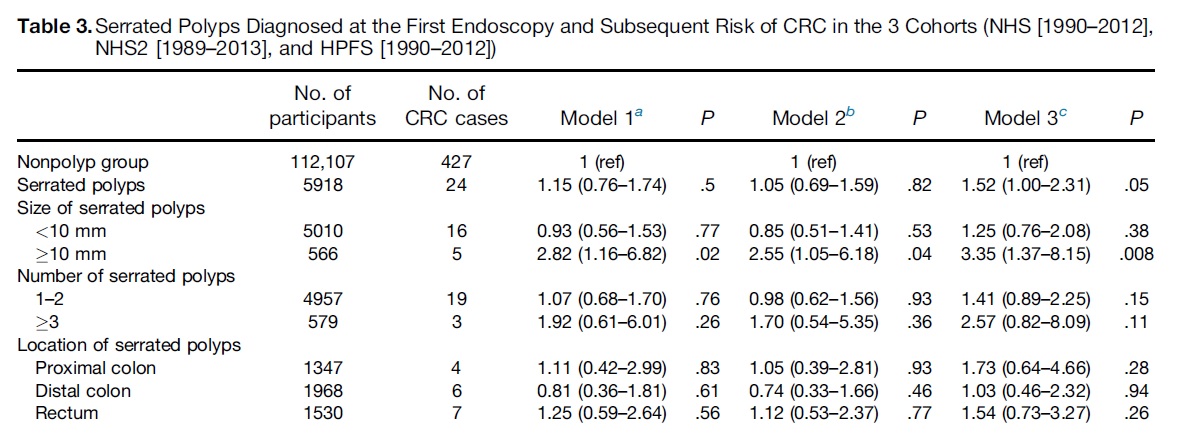
Conv adenoma: 51/6161, SP:24/5918, No polyps:427/112107.
Conv. adenoma group: 32% large lesion. 25% advanced histo. (19& TVA, 4% villous, 2% HGD)
SPs group:10% had at least 1 large SP, 10%>3 SPs #GIJC
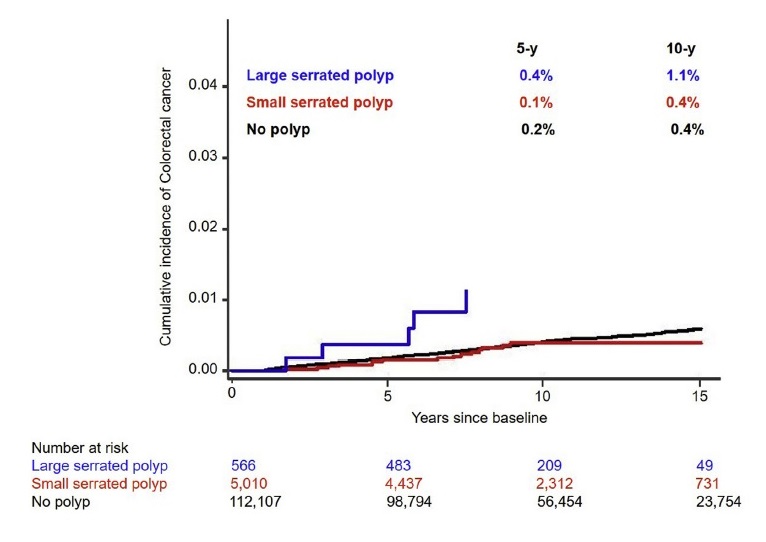
-No polyp: 0.2%/ 0.4%
-Nonadv adneoma:0.1%/ 0.3%
-Adv. adenomas: 0.6%/ 1.7%
-Small SP: 0.1%/ 0.4%
-Large SPs: 0.4%/ 1.1% (all CRC cased dx within 6 yrs)
#GIJC
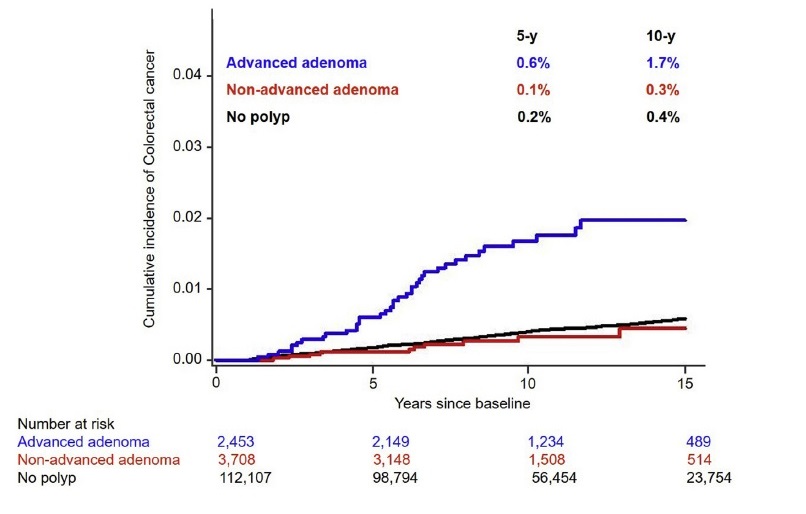
-Compared w/ no polyps, pts w/ advance adenomas had HR of 4.07. No association for non-adv adenoma
-HR for advanced histo: 3.17 for TVA, 8.51 for villous, 5.95 for HGD
-Size & # associated w/ high CRC risk. No risk elevation for 1-2 small adenoma
#GIJC
-Overall high risk. HR 1.52
-Larger SPs HR 3.35. Small SPs> No association.
-No association for # of polyps or sublocation.
> Compared to no polyp group, pts. w/ adenomas and SPs were at high CRC risk. HR 2.69 #GIJC
Compared to other groups:
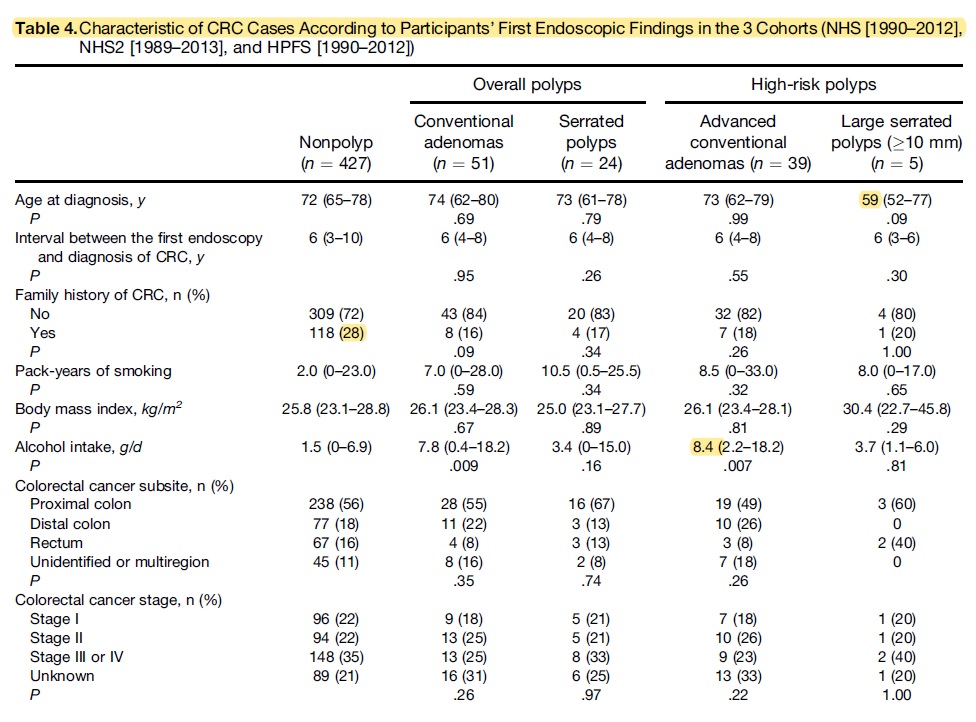
- Pts. w/ large SPs had CRC at a young age (median 59 years)
- CRC in nonpolyp group more likely to have fam history.
- CRC in conv. adenoma drank more alcoholics.
- No diff. in subsite, stage of CRC.
#GIJC
- 4x/3.35x increased CRC risk in advanced adenoma/large SPs> Justifies 3yr surveillance.
- No increased risk in non-adv adenomas or small SPs>
May not require intense surveillance than nonpolyp group
#GIJC
Limitations: unable to distinguish SPs from HPs. Surveillance data were self-reported> measurement error. No info on the quality of endoscopy. Some analyses based on small N.
#GIJC



