1/ This is like the Bat Signal for me... #Tweetorial #Hyponatremia #LoudlyForThePeopleAtTheBackOfTheRoom
https://twitter.com/tonlajr/status/1304011343226437637
2/ The first question in hyponatremia is...
👏Is👏the👏patient👏seizing?👏
If you have a patient with cerebral edema from acute hyponatremia you need to 3% Saline first and ask questions later.
👏Is👏the👏patient👏seizing?👏
If you have a patient with cerebral edema from acute hyponatremia you need to 3% Saline first and ask questions later.
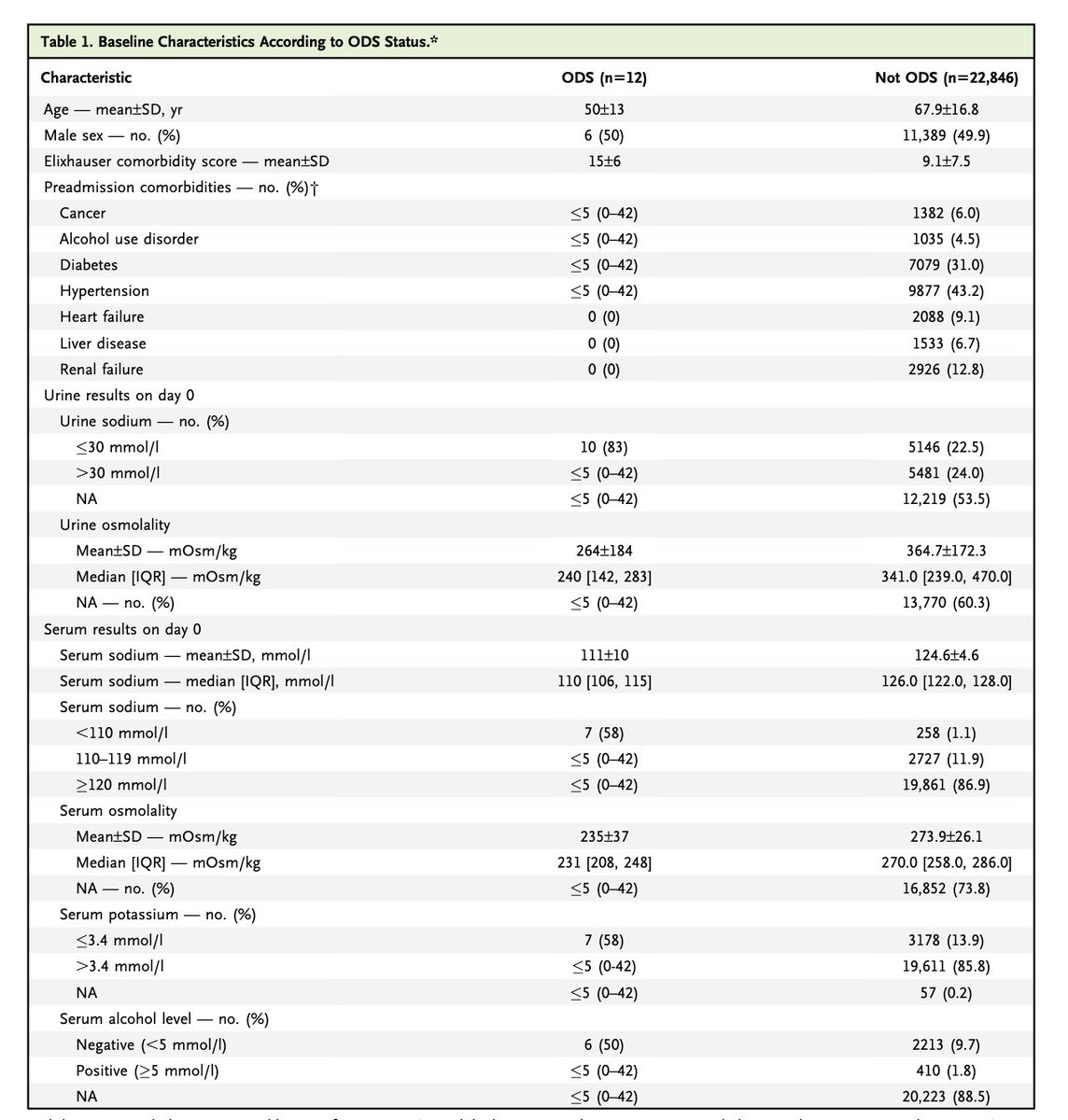
3/ If patients have hyponatremia and have severe symptoms it is 150 ml of 3% then recheck the sodium and give another 150 ml of 3% (I'm using the European guidelines) eje.bioscientifica.com/view/journals/… 
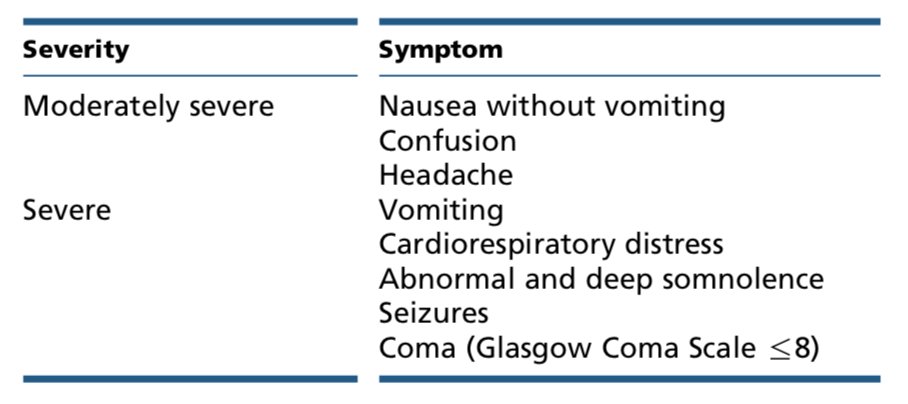
3b/ Be careful with vomiting there 👆🏻
This means if the hyponatremia is causing the vomiting, then you have severe symptoms and it is 3% time. But if the vomiting is causing the hyponatremia, that doesn't automatically indicate severe symptoms and you will need to dig deeper.
This means if the hyponatremia is causing the vomiting, then you have severe symptoms and it is 3% time. But if the vomiting is causing the hyponatremia, that doesn't automatically indicate severe symptoms and you will need to dig deeper.
4/ The goal of acute mgmt is to raise the Na by 5 or stop the symptoms, which ever is quicker. If you have raised the Na by 5 and they are still seizing, then it is probably not the low Na causing the seizure and you need to 👀 deeper. Algorithm from eje.bioscientifica.com/view/journals/… 
5/ But when @tonlajr asked about the approach to sodium he wanted to know abot dx, not acute mgmt so...onward to diagnosis!
6/ I am goin to be walking you through this algorithm:
Step one check the serum osmolarity (and get a repeat sodium, just to make sure it wasn't a lab error)
https://twitter.com/hashamsarwar/status/1304476073627914240?s=20
Step one check the serum osmolarity (and get a repeat sodium, just to make sure it wasn't a lab error)
7/ Since we are looking at a low sodium we expect a low osmolarity (don't worry about the difference between osmolality and osmolarity, anyone who is a stickler about that is being a dick)
If we don't find a low osmolality something weird is going on:
If we don't find a low osmolality something weird is going on:
7b/ Low sodium with a normal osmolarity: Lab error from too much protein (IVIG, multiple myeloma) or too much fat (High lipids or triglys) in the blood. This throws off some lab machines.
(Specifically but not point of care iStats or ABG laboratories)
(Specifically but not point of care iStats or ABG laboratories)
7c/ Low sodium with a high osmolality: this is usually due to hyperglycemia (but can be seen with mannitol, glycine and other edge cases). The hyponatremia is real, but due to another osmotically active particle (glucose in most cases) the are no consequences to the hyponatremia
7/d It is not as simple as that (it never is).
Read this manuscript journal📖: pubmed.ncbi.nlm.nih.gov/26002851/
or listen to this podcast🎧: emcrit.org/emcrit/ed-neph…
Read this manuscript journal📖: pubmed.ncbi.nlm.nih.gov/26002851/
or listen to this podcast🎧: emcrit.org/emcrit/ed-neph…
8/ So that leaves the true hyponatremia. Low sodium and low osmolarity. The branch point here is:
What is the urine osmolarity?
The urine osmolarity tells us if the kidney is causing the hyponatremia or just unable to correct the hyponatremia (despite the best intentions)
What is the urine osmolarity?
The urine osmolarity tells us if the kidney is causing the hyponatremia or just unable to correct the hyponatremia (despite the best intentions)
9/ The urine osmolarity is less than 100 (maybe up to 150 or 200 if the patient has CKD). This indicates a lack of ADH and a kidney that is doing its best to correct the hyponatremia. The problem is not the character of the urine but the amount. Right urine, not enough.
9b/ The differential for low sodium, low serum and urine osmolarity is short:
• Oliguric kidney failure
• Tea and Toast
• Beer Drinkers potomania
• Psychogenic polydipsia
* Recovering from volume depletion hyponatremia
• Oliguric kidney failure
• Tea and Toast
• Beer Drinkers potomania
• Psychogenic polydipsia
* Recovering from volume depletion hyponatremia
9c/ In low Na, low serum and urine osmolarity the urine is getting rid of excess water but the kidney cannot make enough urine because:
• Kidney failure (low GFR)
• T & T / Beer drinkers (lack of solute)
• Psychogen polydipsia (you are drinking faster than you are peeing)
• Kidney failure (low GFR)
• T & T / Beer drinkers (lack of solute)
• Psychogen polydipsia (you are drinking faster than you are peeing)
10 Low sodium, low serum osm, high urine osm. This is ADH dependant hyponatremia. The kidney, stimulated by ADH, is causing the hyponatremia by generating free water. Making more urine here, just makes the Na fall further. 
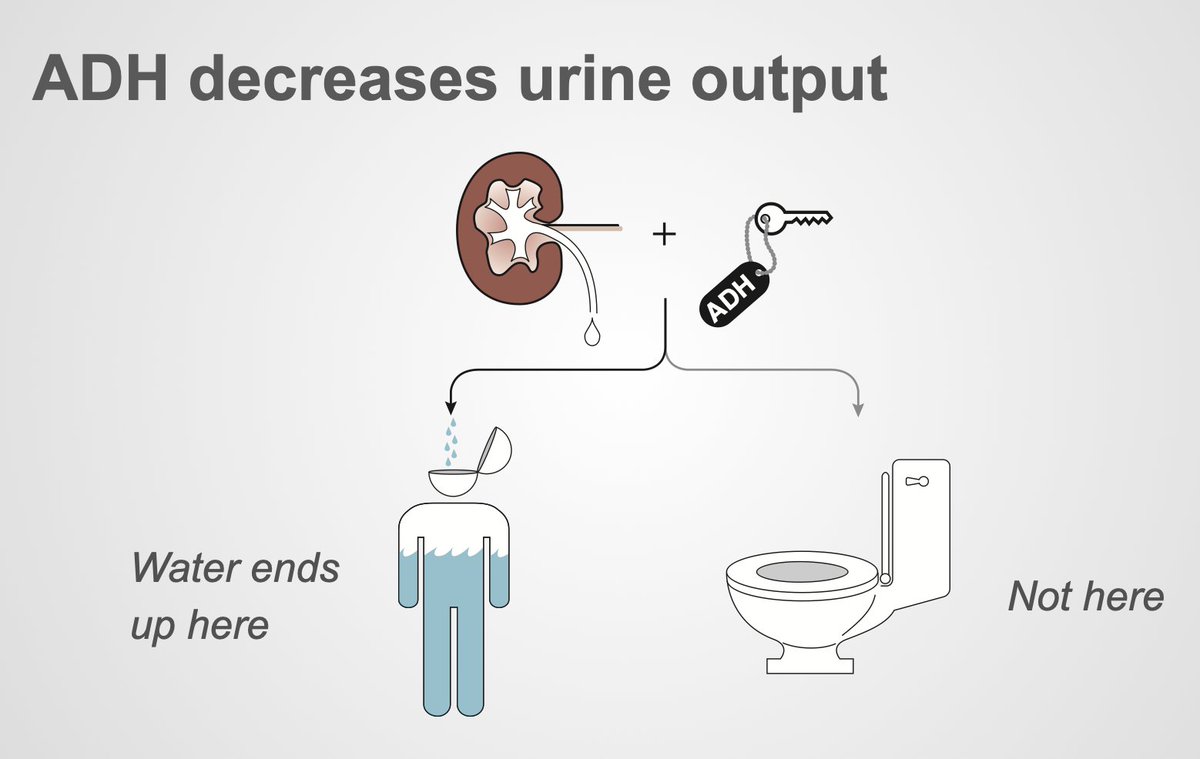
10b/ ADH can be 𝗽𝗵𝘆𝘀𝗶𝗼𝗹𝗼𝗴𝗶𝗰 due to low volume or a perceived low volume state:
Low volume states: GI losses like diarrhea or vomiting; renal losses like diuretics
High volume/low perceived volume: heart failure, liver failure, nephrotic syndrome
Low volume states: GI losses like diarrhea or vomiting; renal losses like diuretics
High volume/low perceived volume: heart failure, liver failure, nephrotic syndrome
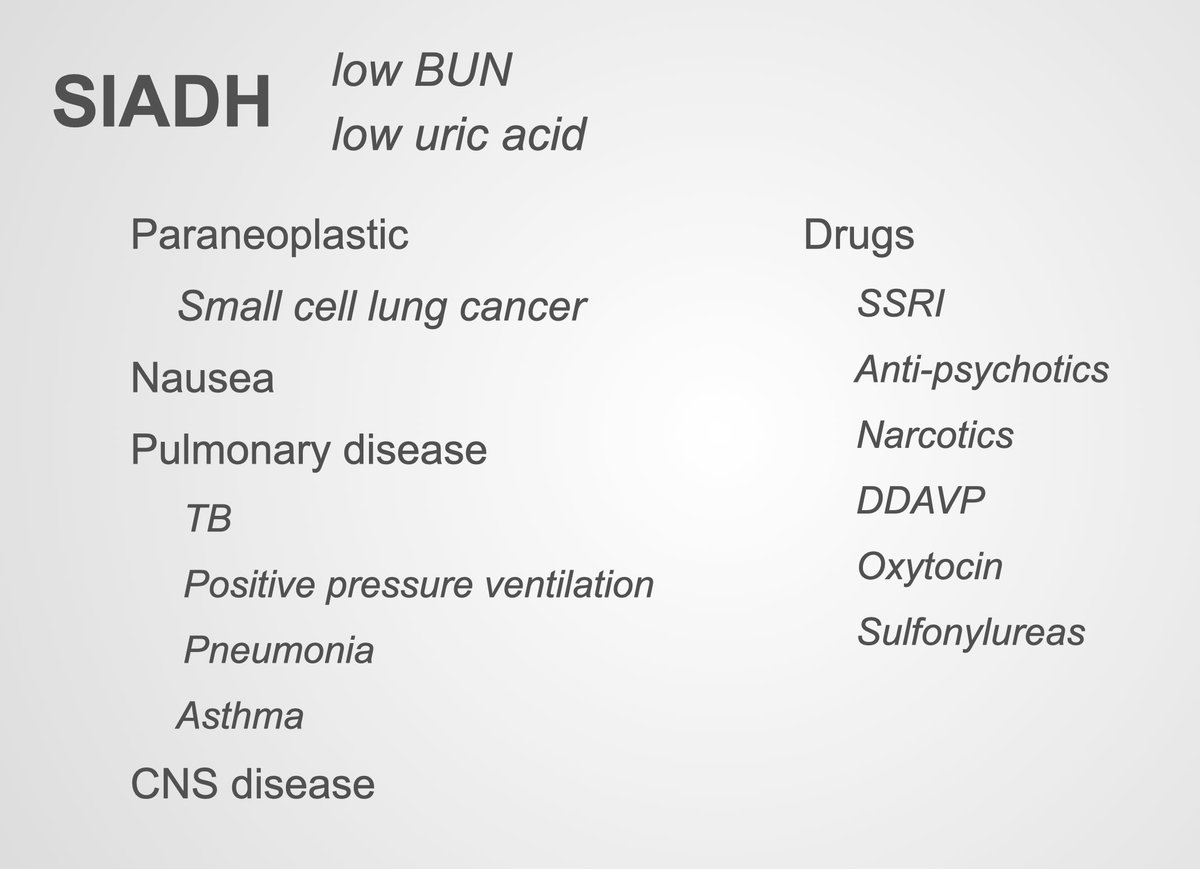
10c/ ADH can be 𝗻𝗼𝗻-𝗽𝗵𝘆𝘀𝗶𝗼𝗹𝗼𝗴𝗶𝗰 (euvolemic):
Adrenal insufficiency
Hypothyroidism (probably doesn't exist, ncbi.nlm.nih.gov/pmc/articles/P…)
SIADH (it's usually this)
Adrenal insufficiency
Hypothyroidism (probably doesn't exist, ncbi.nlm.nih.gov/pmc/articles/P…)
SIADH (it's usually this)
10d/ To differentiate these you can try to use a physical exam to determine volume status but doctors suck at it. pubmed.ncbi.nlm.nih.gov/3674097/ 
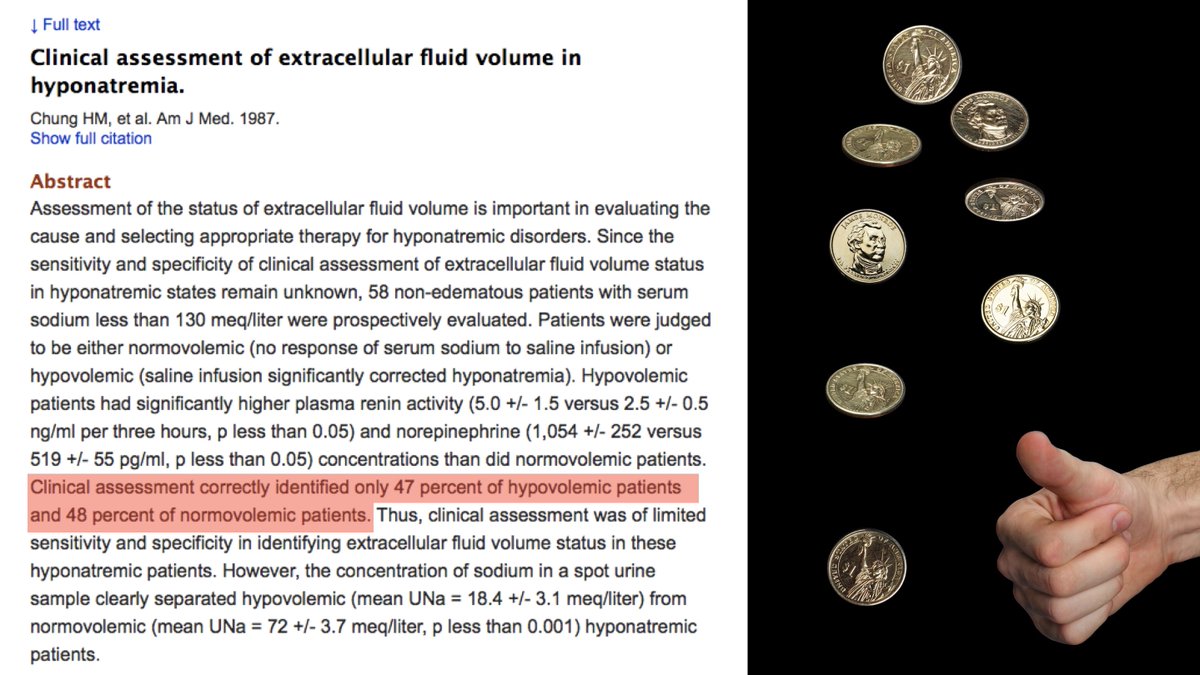
10e/ Instead (or in addition) Check urine sodium and serum uric acid:
Urine sodium low, uric acid high in hypovolemic and hypervolemic hyponatremia
Urine sodium high and uric acid low in euvolemic hyponatremia
Urine sodium low, uric acid high in hypovolemic and hypervolemic hyponatremia
Urine sodium high and uric acid low in euvolemic hyponatremia
• • •
Missing some Tweet in this thread? You can try to
force a refresh