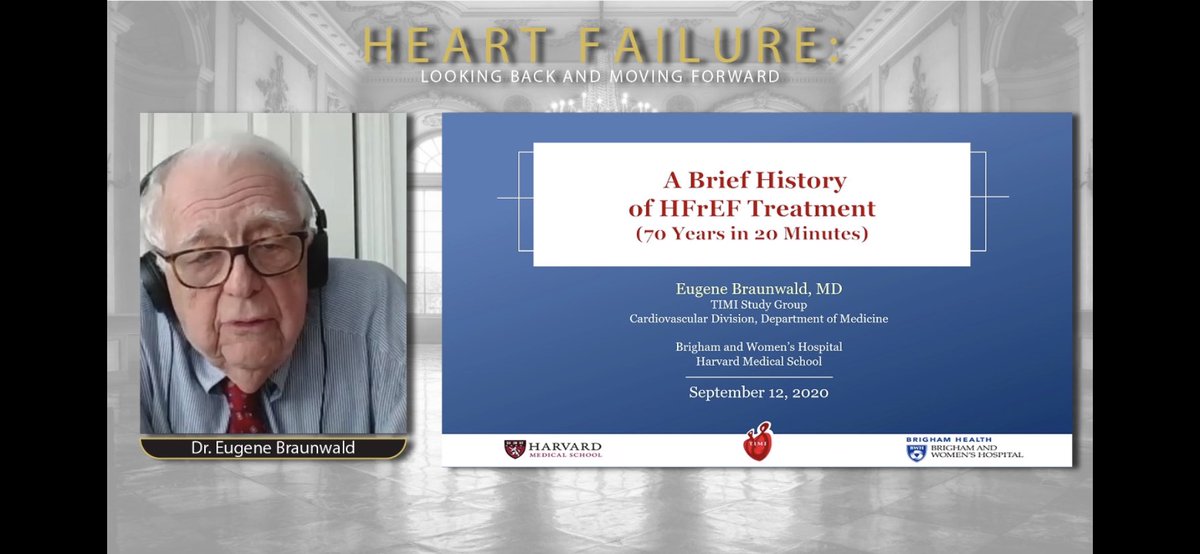
❤️Enjoyed watching the #HeartFailure: Looking Back and Moving Forward webinar.
❤️Dr. Braunwald summarized his 70 years of experience in ~20 minutes.
❤️So much has happened before I was even born!
❤️Yet, so much more to look forward to! Thank you for a tour back in time!



❤️Dr. Braunwald summarized his 70 years of experience in ~20 minutes.
❤️So much has happened before I was even born!
❤️Yet, so much more to look forward to! Thank you for a tour back in time!



❤️I thoroughly enjoyed Dr. John McMurray’s overview of “the five alive” & his emphasis on moving away from vertical integration approach.
❤️Up-titrating each medication should not interfere w/ adding meds w/ complimentary benefits.
❤️No excuses, because #GDMTworks.



❤️Up-titrating each medication should not interfere w/ adding meds w/ complimentary benefits.
❤️No excuses, because #GDMTworks.




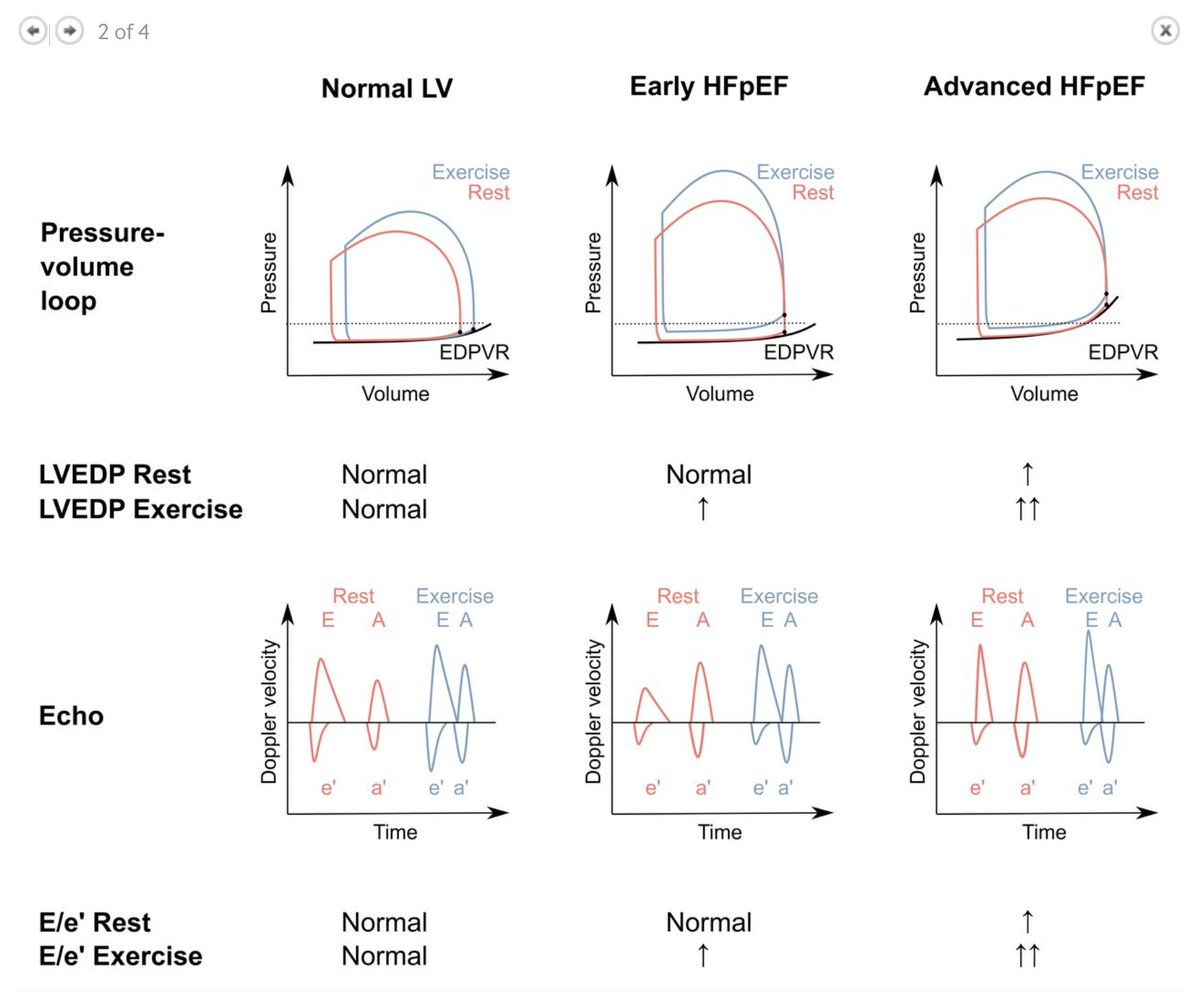
❤️Loved how Dr. Milton Packer went back in time to highlight the origin of LVEF cut-offs & the confusion that followed.
❤️He then advised using strain & myocardial contraction fraction, compared & contrasted common diseases using the same.
❤️HFpEF:disease of something else!



❤️He then advised using strain & myocardial contraction fraction, compared & contrasted common diseases using the same.
❤️HFpEF:disease of something else!




❤️Enjoyed listening to Dr. Lynn Stevenson talk about advances in durable MCS & continued challenges w/ congestion & lack of donor organs.
❤️How can we intervene and interrupt this cascade?
❤️Right heart failure is most commonly the tipping point & we know so little about RV!



❤️How can we intervene and interrupt this cascade?
❤️Right heart failure is most commonly the tipping point & we know so little about RV!




❤️Last but not the least was a fantastic panel discussion re:
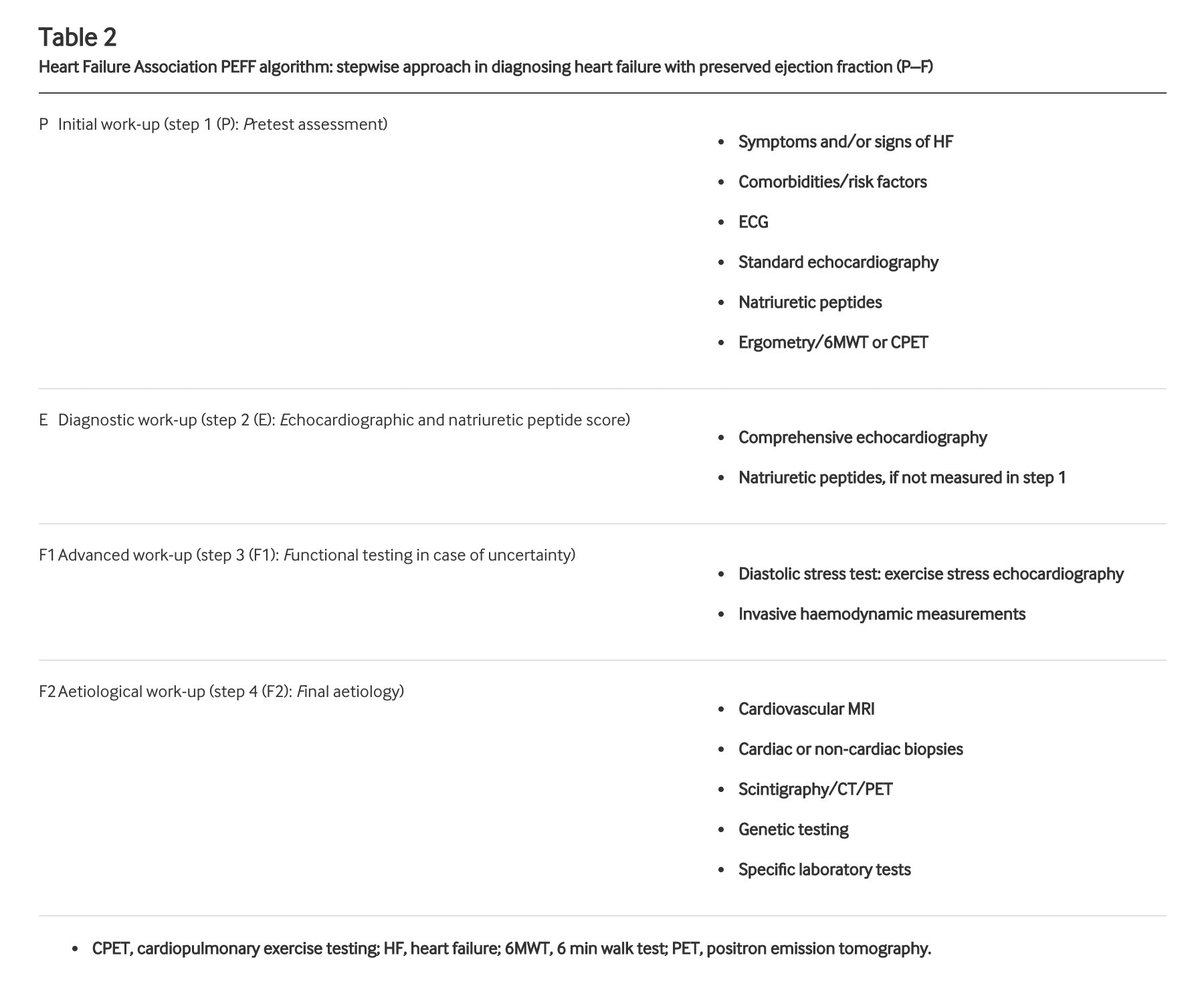
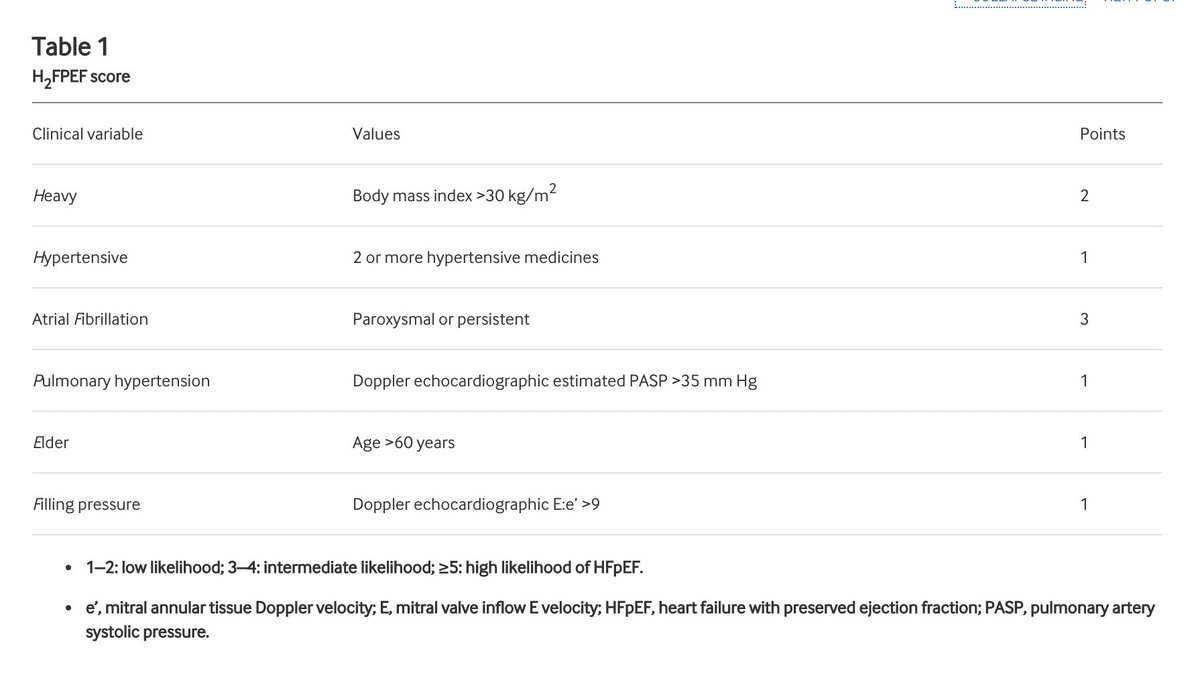
🎯screening for early detection of HF
🎯treat HTN, prevent HF
🎯know more abt RV.
🎯paradigm shift in the way we conduct HF trials—>move away from LVEF?
🎯adopt 💊🧪for diseases causing HFpEF (HCM, amyloidosis etc).
🎯screening for early detection of HF
🎯treat HTN, prevent HF
🎯know more abt RV.
🎯paradigm shift in the way we conduct HF trials—>move away from LVEF?
🎯adopt 💊🧪for diseases causing HFpEF (HCM, amyloidosis etc).
• • •
Missing some Tweet in this thread? You can try to
force a refresh