This thread for people who are interested in CRRT and critical care 😓🤦🏽♂️
Basics about RRT;
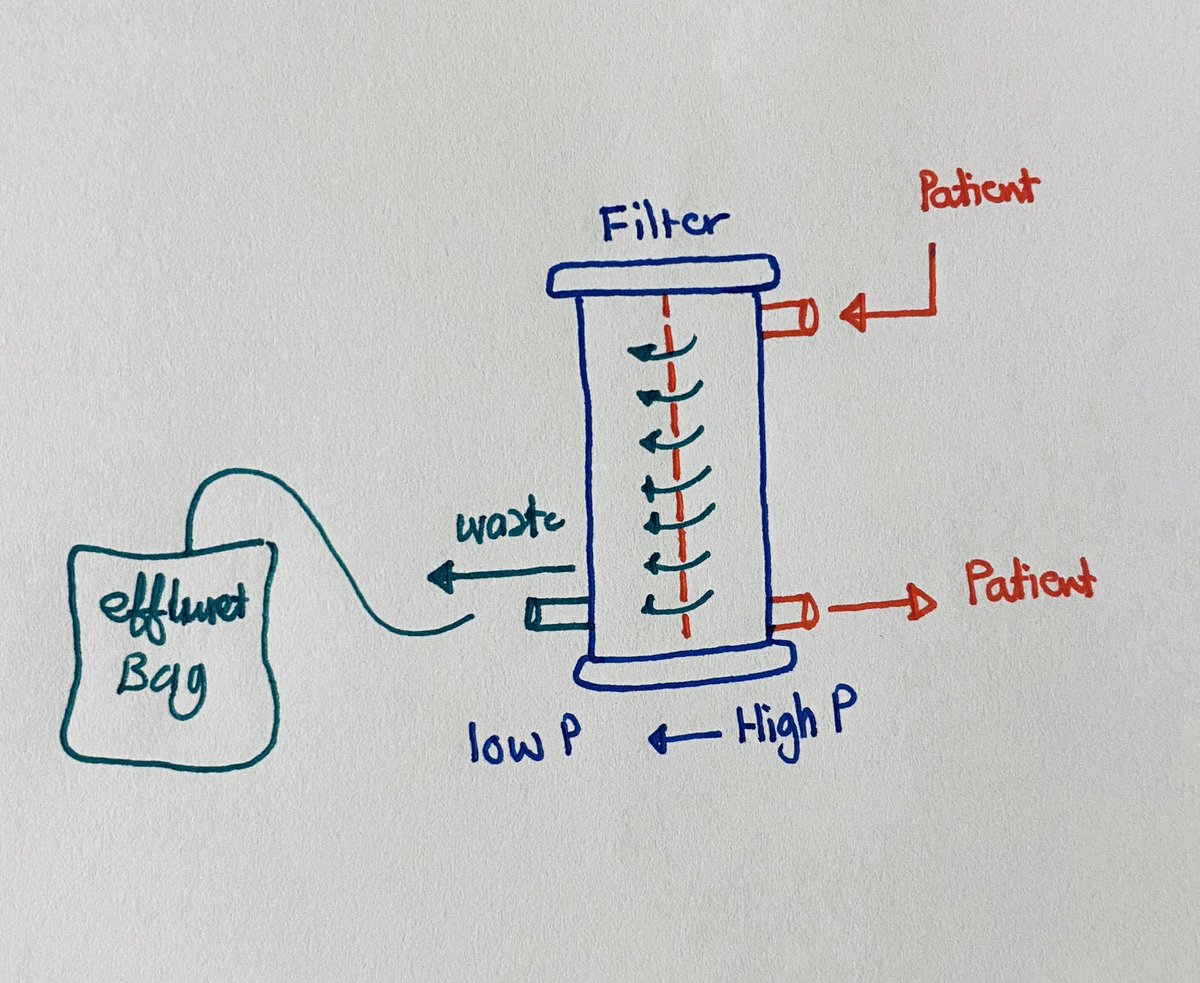
Convection: It depends on Hydrostatic pressure (HP)
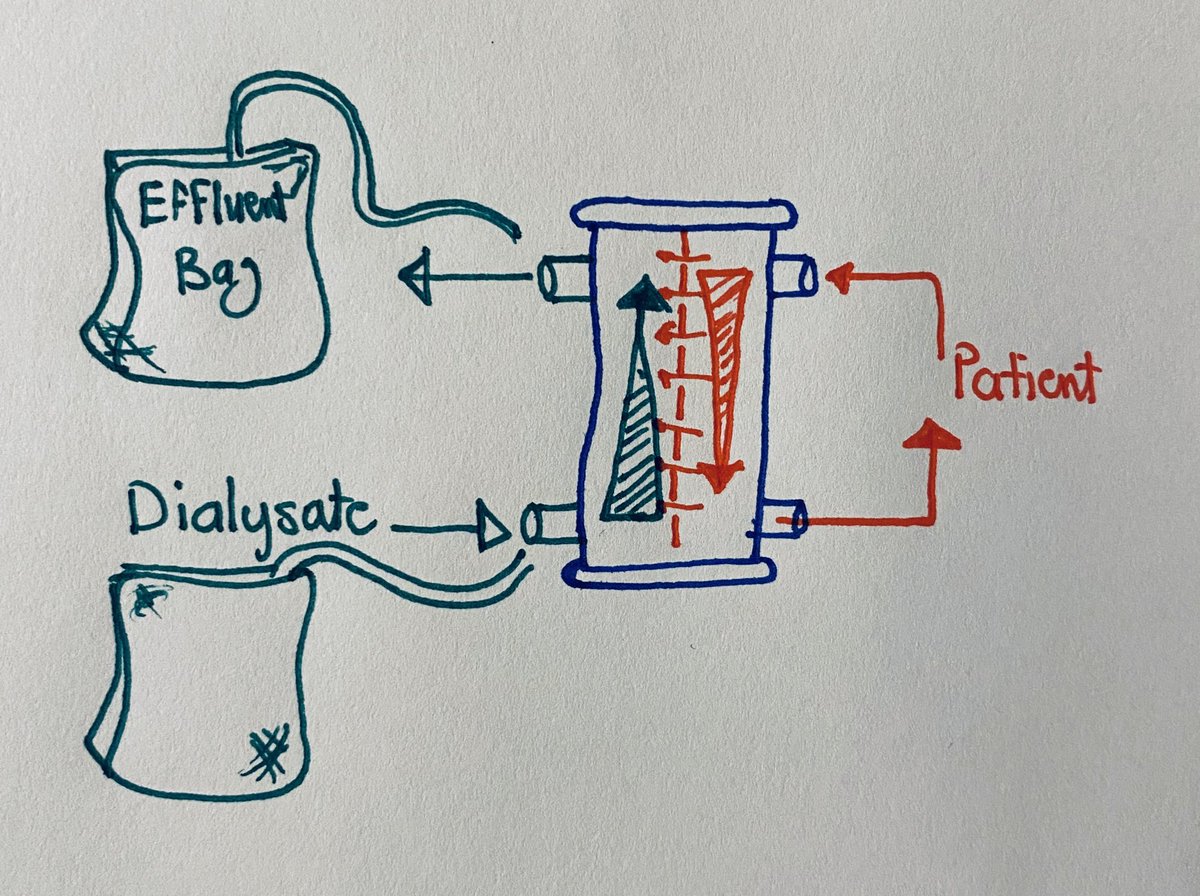
Diffusion: it depends on solutes gradients
Convection: It depends on Hydrostatic pressure (HP)
Diffusion: it depends on solutes gradients
Filtration (Convection): blood from the Pt goes through the filter, In the filter with the effect of HP plasma, small, and medium size molecules get filtered by the HP effect, then the blood goes back to the patient and the filtered fluid and molecules goes to the effluent bag 
Diffusion; blood from the Pt to the filter, In the same time there is another fluid called the Dialysate goes in the opposite way of the filter around the blood which the solutes start the exchange according to the gradient difference and then go out to the effluent bag 
- IHD (Intermittent Hemodialysis)
- SLED (Sustained Low efficiency dialysis)
- SCUF (Slow continues ultrafiltration)
- CVVH (Continues Veno-Venous Hemofiltration)
- CVVHD (Continues Veno-Venous Hemodialysis)
- CVVHDF ( Continues Veno-Venous Hemodiafiltration)
- SLED (Sustained Low efficiency dialysis)
- SCUF (Slow continues ultrafiltration)
- CVVH (Continues Veno-Venous Hemofiltration)
- CVVHD (Continues Veno-Venous Hemodialysis)
- CVVHDF ( Continues Veno-Venous Hemodiafiltration)
IHD, SLED, CVVHD (needs dialysate)
CVVH, SCUF (needs Pressure only)
CVVHDF (needs pressure and dialysate)
Common used mode: CVVHDF
CVVH, SCUF (needs Pressure only)
CVVHDF (needs pressure and dialysate)
Common used mode: CVVHDF
To start Pt on CRRT after reviewing the indications, you need to think about the
• Mode (SLED, SCUF, CVVHD, CVVHF, CVVHDF)
• CRRT Dialyzer membrane,
• type of anticoagulation (None, Heparin, citrate) ,
• substitution fluid
• CRRT dose
• Mode (SLED, SCUF, CVVHD, CVVHF, CVVHDF)
• CRRT Dialyzer membrane,
• type of anticoagulation (None, Heparin, citrate) ,
• substitution fluid
• CRRT dose
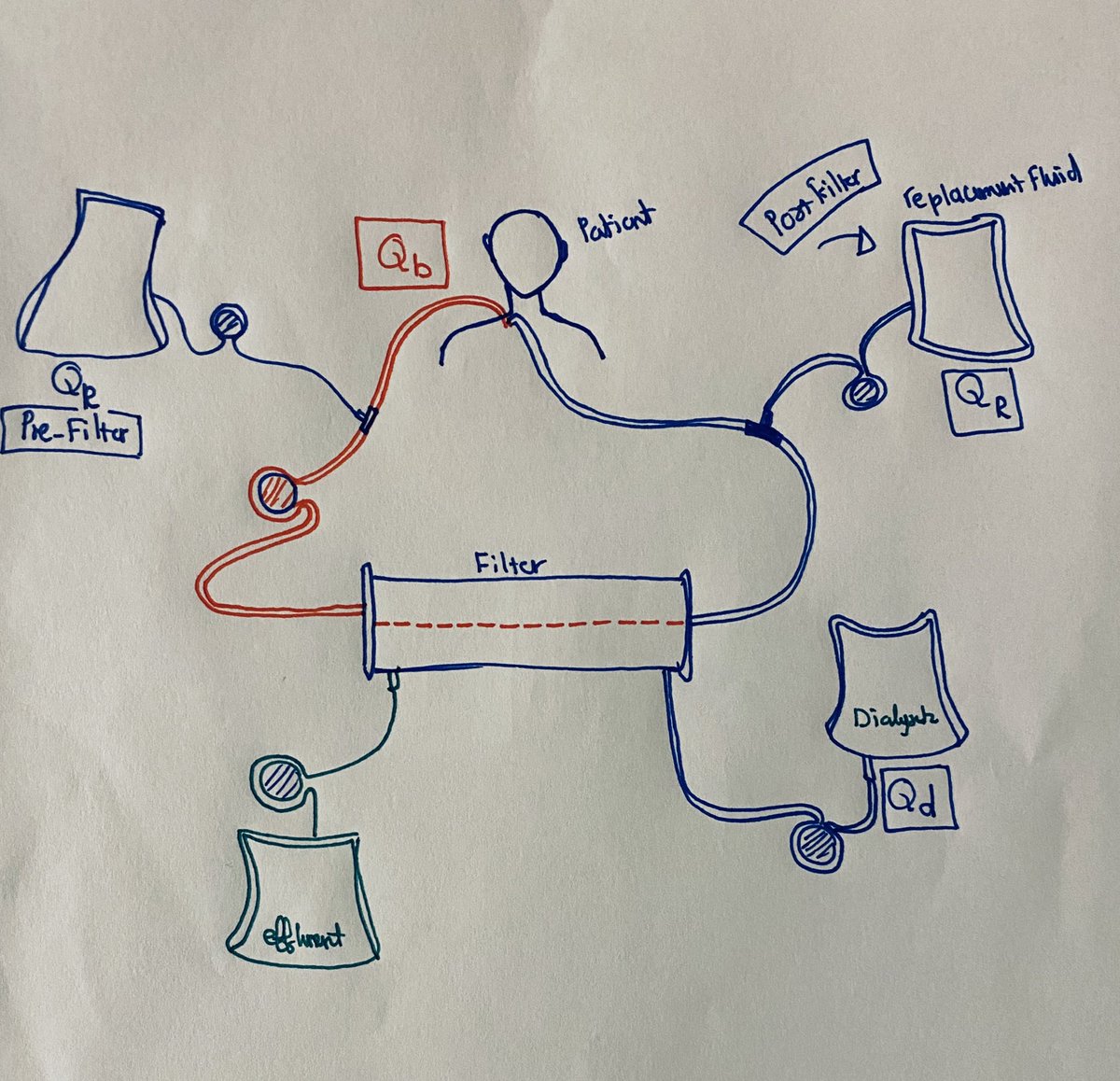
CVVHDF can has Pre-filter, post-filter or pre and post filter replacement fluid
When we think about CVVHDF we need to think about (Blood flow, Replacement fluid, and Dialysate)
Blood flow Qb (ml/min)
Replacement fluid Qr (ml/hr)
Dialysate Qd (ml/hr)
When we think about CVVHDF we need to think about (Blood flow, Replacement fluid, and Dialysate)
Blood flow Qb (ml/min)
Replacement fluid Qr (ml/hr)
Dialysate Qd (ml/hr)
CRRT dose;
20-25 ml/kg/hr (Qd+Qr) 🤯 you can increase according to the metabolic needs
20-25 ml/kg/hr (Qd+Qr) 🤯 you can increase according to the metabolic needs
For example 100 kg patient his [CVVHDF post-filter] dose will be 2000-2500 (Qr + Qd) how can we apply that?
1000 ml/hr for Qd
1000 ml/hr for Qr
Qb ml/min = > 2.5 x Qd
Qb ml/min = > 5 x Qr (post filter)
Qb ml/min = > 6 x Qr (pre filter)
In this pt Qb = > 83 ml/min
1000 ml/hr for Qd
1000 ml/hr for Qr
Qb ml/min = > 2.5 x Qd
Qb ml/min = > 5 x Qr (post filter)
Qb ml/min = > 6 x Qr (pre filter)
In this pt Qb = > 83 ml/min
What’s about the machine pumps limits
Blood Pump 10-450 ml/min
Dialysis and Replacement fluid pump: 0-133 ml/min
Blood Pump 10-450 ml/min
Dialysis and Replacement fluid pump: 0-133 ml/min
What’s about anticoagulation?
You can use Citrate Pre-filter or Systemic Heparin.
If you will use Citrate Pre-filter do not use Pre-filter Qr.
Citrate rate 2 x Qb
You can use Citrate Pre-filter or Systemic Heparin.
If you will use Citrate Pre-filter do not use Pre-filter Qr.
Citrate rate 2 x Qb
Let us take an example;
75 kg Pt who requires CRRT 2/2 resistant metabolic acidosis.
CRRT dose; 75 x 20 = 1500 ml/hr
CVVHD-Post Filter
Qr 750
Qd 750
Qb = 5 x Qr (ml/min) (5 x 12.5)
Qb = > 62 ml/min let’s us say 100
And then re-evaluate according to your metabolic needs
75 kg Pt who requires CRRT 2/2 resistant metabolic acidosis.
CRRT dose; 75 x 20 = 1500 ml/hr
CVVHD-Post Filter
Qr 750
Qd 750
Qb = 5 x Qr (ml/min) (5 x 12.5)
Qb = > 62 ml/min let’s us say 100
And then re-evaluate according to your metabolic needs
What’s about if I want to add citrate ?
As we said Citrate 2 x Qb
Qb is 100 ml/min
Citrate 100 x 2 = 200 ml/hr
Then the final dose will be
Qb 100 ml/min
Citrate 200 ml/hr
Dialysate 750 ml/hr
Qr post filter 550
As we said Citrate 2 x Qb
Qb is 100 ml/min
Citrate 100 x 2 = 200 ml/hr
Then the final dose will be
Qb 100 ml/min
Citrate 200 ml/hr
Dialysate 750 ml/hr
Qr post filter 550
Citrate works by binding to the Ionized Ca in the blood before it reach the filter which it will make it more thin to prevent filter clothing (complications; It needs Ca replacement, and it increases the risk of Citrate toxicity;
Signs of citrate toxicity;
• Rising anion gap, worsening metabolic acidosis
• Falling systemic iCa2+
• Escalating Ca2+ infusion requirements
• Total Ca2+:Systemic iCa2+ Ratio > 2.5:1 (increased Ca2+ gap)
• Rising anion gap, worsening metabolic acidosis
• Falling systemic iCa2+
• Escalating Ca2+ infusion requirements
• Total Ca2+:Systemic iCa2+ Ratio > 2.5:1 (increased Ca2+ gap)
What’s the difference between Pre and Post filter ?
The benefit of pre-filter replacement fluid is diluting the blood which it makes it less clotting risk but less clearance, But the post filter replacement fluid it’s more risk of filter clotting but more clearance.
The benefit of pre-filter replacement fluid is diluting the blood which it makes it less clotting risk but less clearance, But the post filter replacement fluid it’s more risk of filter clotting but more clearance.
What’s about volume removal, it’s mainly driven by the nurse. The nurse will count the fluid in per hr and accordingly you can set up the ultrafiltration rate to reach your goal
For example if your target is 1000 negative in 24 hrs, and your patient on multiple drips and she/he takes total of 300 ml/hr in. Then you set the UF rate 350 ml/hr then your Pt will have 50 ml negative every hr.
Things you need to watch on CRRT;
• Acsess site
• Pump Alarms
• Filtration fraction
• and TMP
• Acsess site
• Pump Alarms
• Filtration fraction
• and TMP
Keep Filtration fraction (FF) < 20% and TMP < 300 to avoid early filter clothing
FF = In none CRRT Pt = GFR/RPF
FF = total UFR/Qb x 100%
TMP = Transmembranous pressure = [(filter P + Return P)/2]-Effluent pressure
FF = In none CRRT Pt = GFR/RPF
FF = total UFR/Qb x 100%
TMP = Transmembranous pressure = [(filter P + Return P)/2]-Effluent pressure
We have 4 different pressure alarms;
The blood pump pressure Pa, Filter pressure Pf, Effulent pressure Pe, and Return pressure Pr.
The blood pump pressure Pa, Filter pressure Pf, Effulent pressure Pe, and Return pressure Pr.
Blood pump access alarm 🚨
- check the catheter position
- The blood flow number might be high
The pressure at the outgoing line to patient (Pr)is high?!
- check the catheter line and positioning
- check the catheter position
- The blood flow number might be high
The pressure at the outgoing line to patient (Pr)is high?!
- check the catheter line and positioning
Always try to keep the difference between the Pf and Pr is < 100 means the Pf-Pr = < 100 to prevent filter Clotting
The pressure in the filter is high (TMP) equals= [(Pf+Pr)/2]-Pe always try to keep it < 300 to prevent filter Clotting.
The pressure in the filter is high (TMP) equals= [(Pf+Pr)/2]-Pe always try to keep it < 300 to prevent filter Clotting.
But it’s not that easy this is just the basics, there a lot more on CRRT and electrolytes
If you have any questions please ask @Yahyaraufahmad
• • •
Missing some Tweet in this thread? You can try to
force a refresh