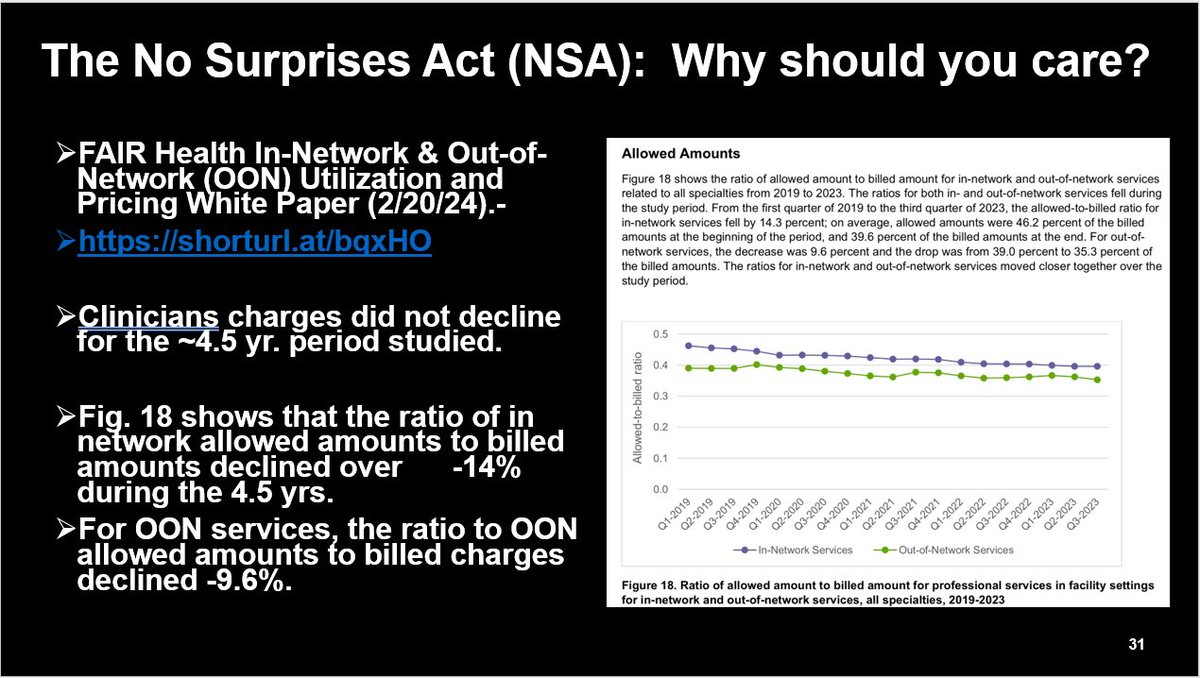
1/ So the #TX health plans--after supporting the solution to #surprisemedicalbilling which passed unanimously--are now pointing fingers--lets consider the facts--1. per the TX Dept. of Insurance (TDI), when clinicians informally settle their dispute before the formal dispute ....
2/ resolution process (IDR), the plans are settling for 4X of the original reimbursement paid; when clinicians go thru the IDR process, the independent dispute adjudicator is awarding >5.3X of the plan's initial reimbursement--based on TDI's report of the 1st 6 months--see charts
3/ So the original plan reimbursements are unreasonably low--one could reasonably conclude--so low that the plans are willing to pay 4X in settlement before IDR--& the Pts are protected & removed from the IDR process--the statutory factors for determining the final $ are strong 



4/ but fair--& both sides must pay 4 the costs of IDR--not loser pays--& only $5K in any 1 dispute 4 batching of claims--hardly a 1 sided solution--no, @txhealthplans your original instinct in supporting SB 1264 was right--don't complain now when your members have to pay fairly
5/ @KHancock4TX @TomOliverson @TCEP @drdanchoi @sonodoc99 @fuzzymittens @ACEPNow @813JAFERD @RichDuszak @reh3md @amychomd @Reese_Tassey @ercoderguy @movinmeat @ASAGrassroots @RadiologyACR @michelekimball @GrassrootsEM @MichStateMedSoc @ahahospitals @AmerMedicalAssn @mass_marion
• • •
Missing some Tweet in this thread? You can try to
force a refresh