We must protect the vulnerable in our communities from SARS-CoV-2. It is our responsibility more than theirs, because the primary means to protect them is for the rest of us to suppress transmission of the virus and keep circulating virus at very low levels. 1/8 

If we look back to March through to June, the number of cases in any given county in people aged 65 and older correlates with the number of sporadic cases in the community. High levels of virus in the community increase the risk for older and other vulnerable people. 2/8 

This is a lethal virus, and mortality rises quickly with age. The case-fatality rate for those cases reported March to June was 0.2% in those aged 20-39, but 33% in those 85 and above. 3/8 

We know from our SCOPI sero-prevalence study that back then we were detecting one in three cases, and our testing was biased to those with severe disease, so now we would expect hospitalization and fatality rates to be less than one-third of what we saw in March and April. 4/8
Our best estimate of infection-fatality ratio at present is that it ranges from around 0.1% in those aged 20-30 to 7-8% in those aged 85 and older. If we fail to protect the elderly, we may expect 4-6% mortality in those cases aged 65 years and older through the winter. 5/8
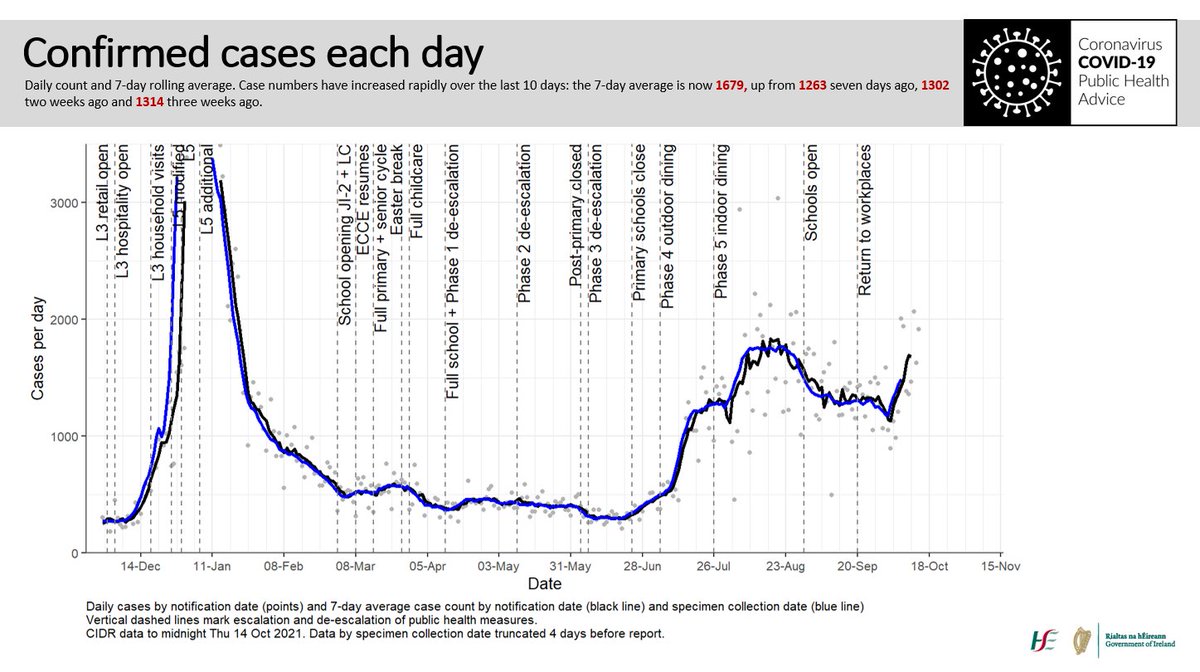
The recent rise in cases in Ireland started in younger age groups with very mild disease, but now we are seeing rising cases in older people, hospitalisations and deaths. We had 4 deaths with COVID-19 in all of August, and 18 so far in September. 6/8 

There are those who are saying we are not seeing hospitalisations or deaths in this phase of the pandemic. We are, sadly. They are delayed, and now occurring at the rates that we would have expected. They will rise further if we don’t act now. 7/8
This is why I limit my social contacts, avoid congregation and crowded spaces, wash my hands, keep my distance, wear a face covering. If I don’t, I constrain and risk the lives of valuable, valued, but vulnerable members of our society. 8/8
• • •
Missing some Tweet in this thread? You can try to
force a refresh