While on the topic on #Angioedema with @EMBoardBombs
It was mentioned about tPA causing angioedema. It is scary and happened to me. I didn't know about it until it happened to me.
Follow along for a short #medtweetorial case report with some tips. ncbi.nlm.nih.gov/pmc/articles/P…
It was mentioned about tPA causing angioedema. It is scary and happened to me. I didn't know about it until it happened to me.
Follow along for a short #medtweetorial case report with some tips. ncbi.nlm.nih.gov/pmc/articles/P…

The most dreaded adverse effect of tPA, hemorrhagic conversion of an ischemic stroke.
But there is another scary, unusual & potentially life-threatening adverse effect of tPA. ANGIOEDEMA
It usually affects the side of the tongue ipsilateral to the stroke.
But there is another scary, unusual & potentially life-threatening adverse effect of tPA. ANGIOEDEMA
It usually affects the side of the tongue ipsilateral to the stroke.
The patient in the picture presented with left side weakness/facial droop and his stroke was on the right brain. Hence the left-sided tongue swelling.
What is Angioedema?
It is an acute well-demarcated swelling involving the deeper layers of skin of the skin.
What is Angioedema?
It is an acute well-demarcated swelling involving the deeper layers of skin of the skin.
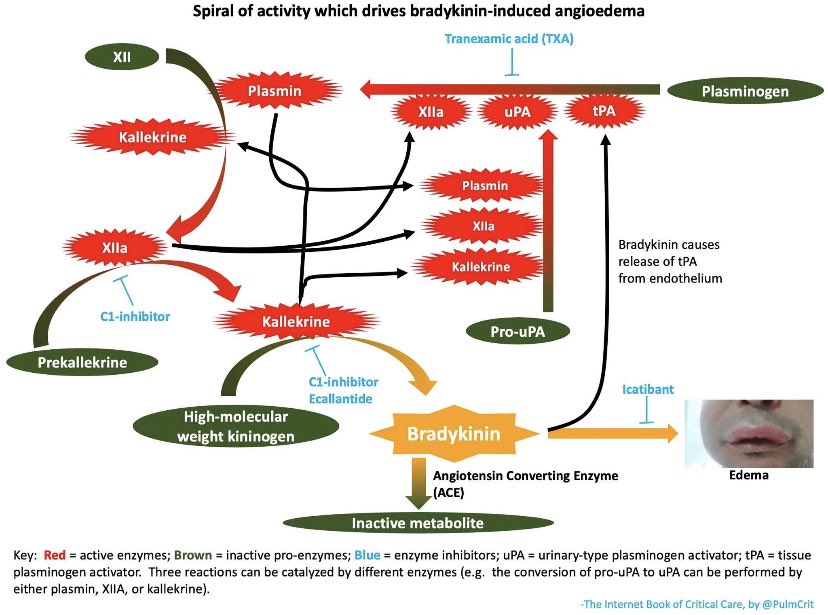
The increase in plasmin may play a role by activating the
kinin pathway ⏭️ to the formation of the vasodilator
bradykinin.
Plasmin also activates the complement system
and leads to the production of C3a, C4a, & C5a, which also cause mast cell degranulation and histamine release
kinin pathway ⏭️ to the formation of the vasodilator
bradykinin.
Plasmin also activates the complement system
and leads to the production of C3a, C4a, & C5a, which also cause mast cell degranulation and histamine release
It usually affects the face, genitalia, as well as
the upper respiratory airways & the intestinal epithelial
lining & can cause abd pain/diarrhea
Angioedema can 2/2 a hereditary deficiency
in C1-esterase or an allergic reaction to
some medications, MCC ACE inhibitors
the upper respiratory airways & the intestinal epithelial
lining & can cause abd pain/diarrhea
Angioedema can 2/2 a hereditary deficiency
in C1-esterase or an allergic reaction to
some medications, MCC ACE inhibitors
The half-life of tPA is approximately seven minutes; therefore, the risk of angioedema can still occur after the infusion has stopped.
But why does this happen?
tPA hydrolyzes plasminogen to plasmin & this results
in its fibrinolytic effect.
But why does this happen?
tPA hydrolyzes plasminogen to plasmin & this results
in its fibrinolytic effect.
How often does this happen?
A prospective study examining176 patients treated w/ tPA for acute ischemic stroke and found evidence of orolingual angioedema in 9 patients (5.1%)
Thankfully the reaction is typically mild and transient unless they are on an ACE
A prospective study examining176 patients treated w/ tPA for acute ischemic stroke and found evidence of orolingual angioedema in 9 patients (5.1%)
Thankfully the reaction is typically mild and transient unless they are on an ACE
Why does this happen on the contralateral side?
It is thought that the lateralization of the edema was hypothesized to be due to the loss of autonomic innervation of that side
It is thought that the lateralization of the edema was hypothesized to be due to the loss of autonomic innervation of that side
The initial goal of therapy is airway management w/ early intubation if necessary.
The most skilled person available must handle airway
interventions.
The tPA infusion should be stopped.
Tx w/ histamine antagonists, diphenhydramine along
with corticosteroids.
The most skilled person available must handle airway
interventions.
The tPA infusion should be stopped.
Tx w/ histamine antagonists, diphenhydramine along
with corticosteroids.
As pointed out by @PulmCrit TPA causes bradykinin-mediated angioedema, so antihistamine/steroid wont work if it’s truly a bradykinin mediated process. if anything works for this, it might be tranexamic acid +/- bradykinin pathway inhibitors 
One of the main reasons most of us still give all the typical meds for “histamine mediated anaphylaxis” is that in the moment you don’t how much or little is histamine related or not. Am I wrong here? Would love your feedback @PulmCrit
I still feel like most of my colleagues now and in residency still treated suspected bradykinin mediated angioedema with the H blockers and steroids and epi bc of that. @blakebriggsMD thoughts?
• • •
Missing some Tweet in this thread? You can try to
force a refresh






