1/ How can we reduce Medicare spending without harming patients?
What we do @AledadeACO is transformative, but hard.
There are some low hanging fruit. This was one of them
Prior auth for repetitive, scheduled non-emergency ambulance transportation
cms.gov/newsroom/press…
What we do @AledadeACO is transformative, but hard.
There are some low hanging fruit. This was one of them
Prior auth for repetitive, scheduled non-emergency ambulance transportation
cms.gov/newsroom/press…
2/ When CMS first released their public use files, I ran some analyses looking for aberrations-
One thing that jumped right out was...Repetitive non-emergency ambulance runs- often for the same person going back and forth to dialysis 3 times a week.
One thing that jumped right out was...Repetitive non-emergency ambulance runs- often for the same person going back and forth to dialysis 3 times a week.
https://twitter.com/Farzad_MD/status/454069078081433601?s=20
3/ In my blog @BrookingsInst back in 2014 I wrote:
"Medicare and law enforcement officials will need to create new processes for dealing with a potential flood of outlier reports from amateur sleuths like me."
But prevention >> fraud enforcement
brookings.edu/blog/up-front/…
"Medicare and law enforcement officials will need to create new processes for dealing with a potential flood of outlier reports from amateur sleuths like me."
But prevention >> fraud enforcement
brookings.edu/blog/up-front/…
4/ Later in 2014, @CMSinnovates launched an experiment to see if prioir authorization for these repetitive scheduled non-emergent ambulance transports (RSNAT, natch) would reduce costs without harming beneficiaries.
(private insurance companies do this as a matter of course)
(private insurance companies do this as a matter of course)
5/ They started in the areas known to be problematic. I'm sure the mob is somehow involved in the NJ shenanigans, they are so brazen. Also PA and SC.
Over a quarter of all RSNATs had been improper, according to the @OIGatHHS and unsurprisingly, putting in controls worked!
Over a quarter of all RSNATs had been improper, according to the @OIGatHHS and unsurprisingly, putting in controls worked!
6/ Another demonstration with prior auth for durable medical equipment also found significant savings without patient harm.
Medicare needs to be able to do reforms like this, and @CMSinnovates gives it the ability to implement them without special interest lobbying blocking them
Medicare needs to be able to do reforms like this, and @CMSinnovates gives it the ability to implement them without special interest lobbying blocking them
7/ so...only 6 years later, we have the second interim evaluation showing cost savings in the initial plus expanded demonstration states, and CMS is expanding this nationwide.
I wish it could happen faster, but this is why @CMSinnovates need to stay
innovation.cms.gov/data-and-repor…
I wish it could happen faster, but this is why @CMSinnovates need to stay
innovation.cms.gov/data-and-repor…
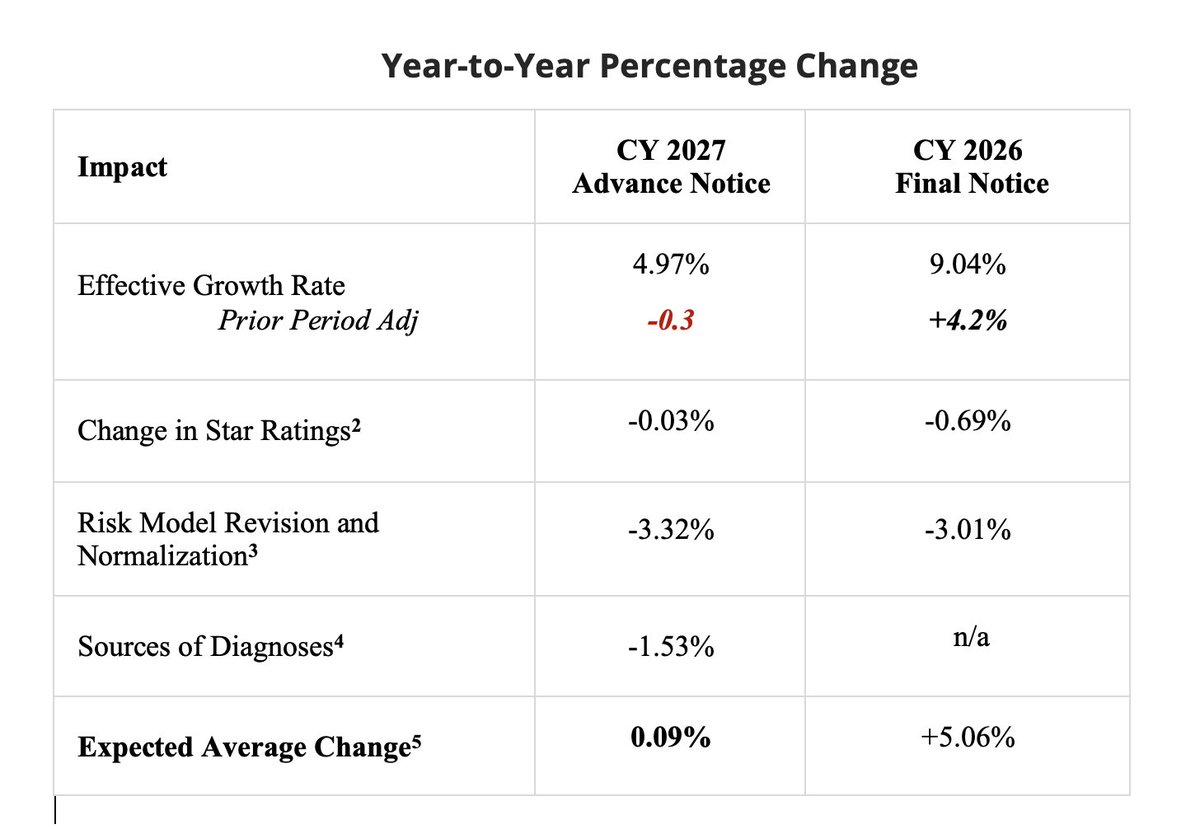
8/ So here's the data you came for.
When you have large effect sizes you don't need very fancy analytics, though they did them anyway,
The high outlier initial states fell down immediately to below comparison states.
The second wave also dropped, albeit they had less to shed
When you have large effect sizes you don't need very fancy analytics, though they did them anyway,
The high outlier initial states fell down immediately to below comparison states.
The second wave also dropped, albeit they had less to shed

9/ So what was the compensatory care (there is *always* a put for every take)?
More home health services. Turns out a lot of those patients didn't need to be put on an ambulance 3x a week. Care could go to their home (including home dialysis)
I will take that.
More home health services. Turns out a lot of those patients didn't need to be put on an ambulance 3x a week. Care could go to their home (including home dialysis)
I will take that.

10/ But inevitably people will say "limiting care must have tradeoffs! someone is going to be harmed if we don't keep paying for these without question."
Maybe @tradeoffspod will do an episode on this, cause you have to squint hard to find it.
LOWER prob of ED/Hospital use
Maybe @tradeoffspod will do an episode on this, cause you have to squint hard to find it.
LOWER prob of ED/Hospital use

11/ Also interesting that this didn't create an ongoing large burden of bureaucracy.
About half of the ambulance companies, esp those that depended on these routine transports went out of business.
The rate of denials went down back to baseline after a few quarters.

About half of the ambulance companies, esp those that depended on these routine transports went out of business.
The rate of denials went down back to baseline after a few quarters.


12/ In conclusion,
There are lots of little things we can do to reduce waste in Medicare, and we should do them
CMMI is a good thing
I wish it wouldn't take so long to go from pilot to policy.
(but nice job on the eval @kcontreary)
There are lots of little things we can do to reduce waste in Medicare, and we should do them
CMMI is a good thing
I wish it wouldn't take so long to go from pilot to policy.
(but nice job on the eval @kcontreary)
• • •
Missing some Tweet in this thread? You can try to
force a refresh