Excited to share this new COVID modeling script:
It applies various age-stratified IFR estimates to calculate the expected overall IFR in a given country. It's based on demographics (countries population pyramids): github.com/mbevand/covid1…
Many interesting findings—read on
1/n
It applies various age-stratified IFR estimates to calculate the expected overall IFR in a given country. It's based on demographics (countries population pyramids): github.com/mbevand/covid1…
Many interesting findings—read on
1/n
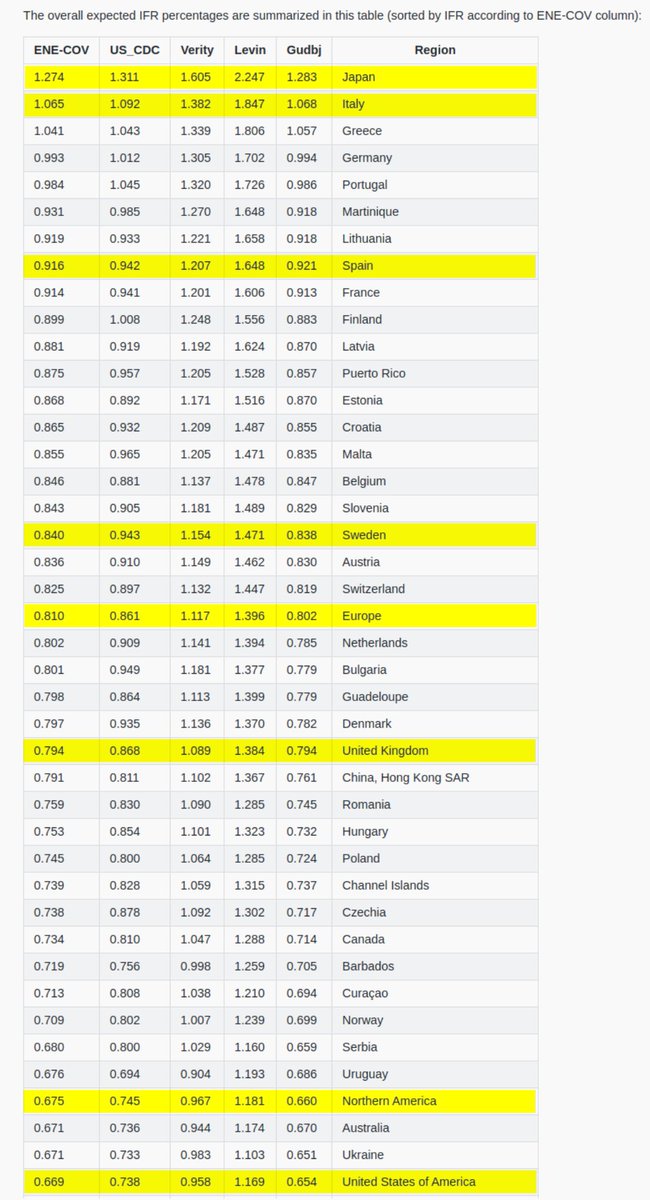
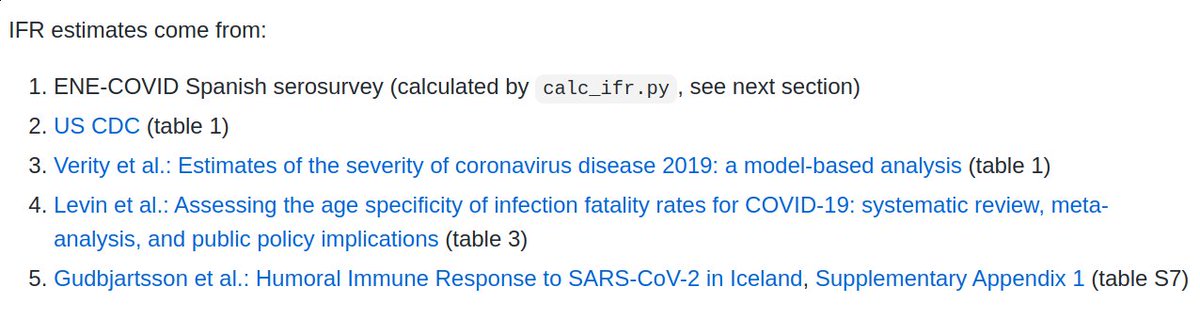
First off, I use five different sources estimating the age-stratified Infection Fatality Ratio of COVID-19:
1. ENE-COVID
2. US CDC
3. Verity et al.
4. Levin et al.
5. Gudbjartsson et al.
If you know of more sources, let me know and I'll add them to my script
2/n
1. ENE-COVID
2. US CDC
3. Verity et al.
4. Levin et al.
5. Gudbjartsson et al.
If you know of more sources, let me know and I'll add them to my script
2/n
So, what do we find?
The overall IFR estimates, with the exception of Levin et al., are relatively consistent with each other, usually within 30-40%. Levin et al. is up to 2-fold higher than the others, depending on the country.
3/n
The overall IFR estimates, with the exception of Levin et al., are relatively consistent with each other, usually within 30-40%. Levin et al. is up to 2-fold higher than the others, depending on the country.
3/n
The country with the oldest population is expected to have the highest overall IFR: Japan at 1.3-1.6% (excluding Levin et al.)
The one with the youngest pop. is expected to have the lowest overall IFR: Uganda at 0.074-0.147%
>10-fold difference between these 2 countries!
4/n
The one with the youngest pop. is expected to have the lowest overall IFR: Uganda at 0.074-0.147%
>10-fold difference between these 2 countries!
4/n
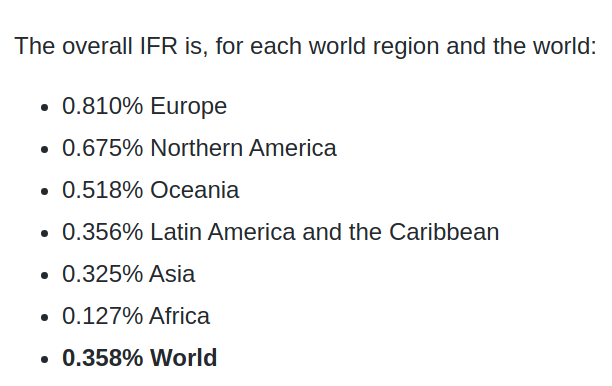
In fact, the young age of the population of Africa is a major factor explaining their small number of deaths. We find IFR=0.13-0.24% for Africa, compared to IFR=0.8-1.4% in Europe, a ~5-fold difference!
5/n
5/n
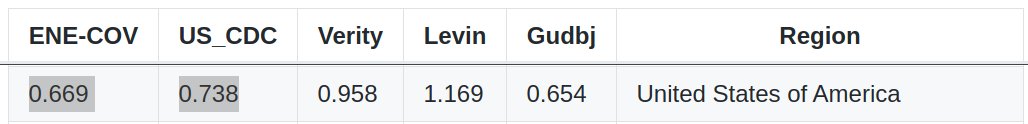
Using ENE-COVID data from June 2020, our code accurately predicts an overall IFR of 0.669% in the United States.
This is very close to the last 2 estimates from the US CDC:
- 0.65% published in July 2020 web.archive.org/web/2020071205…
- 0.738% calculated from their Sep 2020 update
6/n
This is very close to the last 2 estimates from the US CDC:
- 0.65% published in July 2020 web.archive.org/web/2020071205…
- 0.738% calculated from their Sep 2020 update
6/n
Here's a summary of the expected overall IFR for each continent.
The youngest continents should fare the best, thanks to their young population:
8/n
The youngest continents should fare the best, thanks to their young population:
8/n
Finally, the real-world overall IFR will dependent on many factors: varying prevalence among age groups, underlying health conditions, access to healthcare, socioeconomic status, ethnicity, etc.
But I expect the age of the population to be one of the most important factors.
9/n
But I expect the age of the population to be one of the most important factors.
9/n
• • •
Missing some Tweet in this thread? You can try to
force a refresh






