People are travelling abroad for plastic surgery procedures. In some cases there has bee injury or death. There can be issues of lack of regulation and insurance. Today I'm chairing a PEOPIL webinar to consider the issues presented. Great line up of speakers
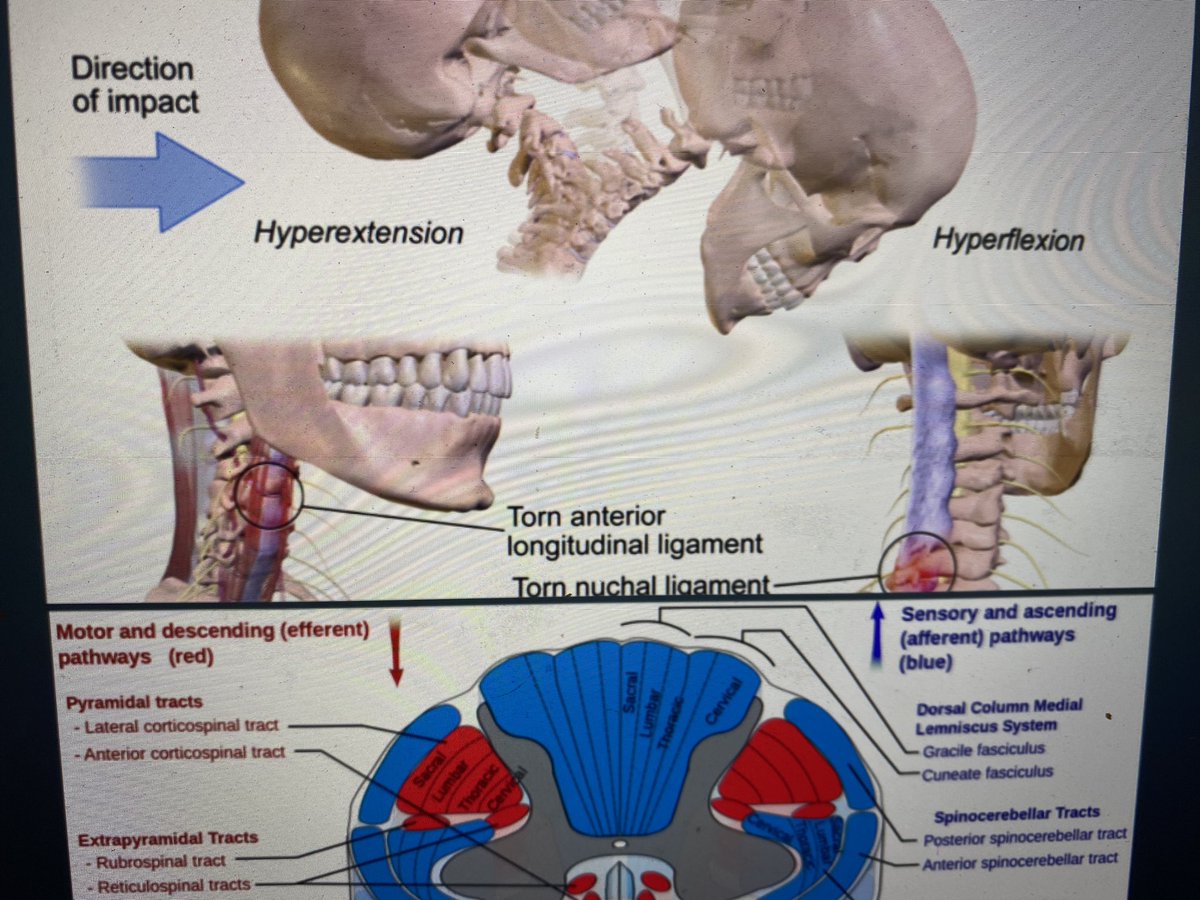
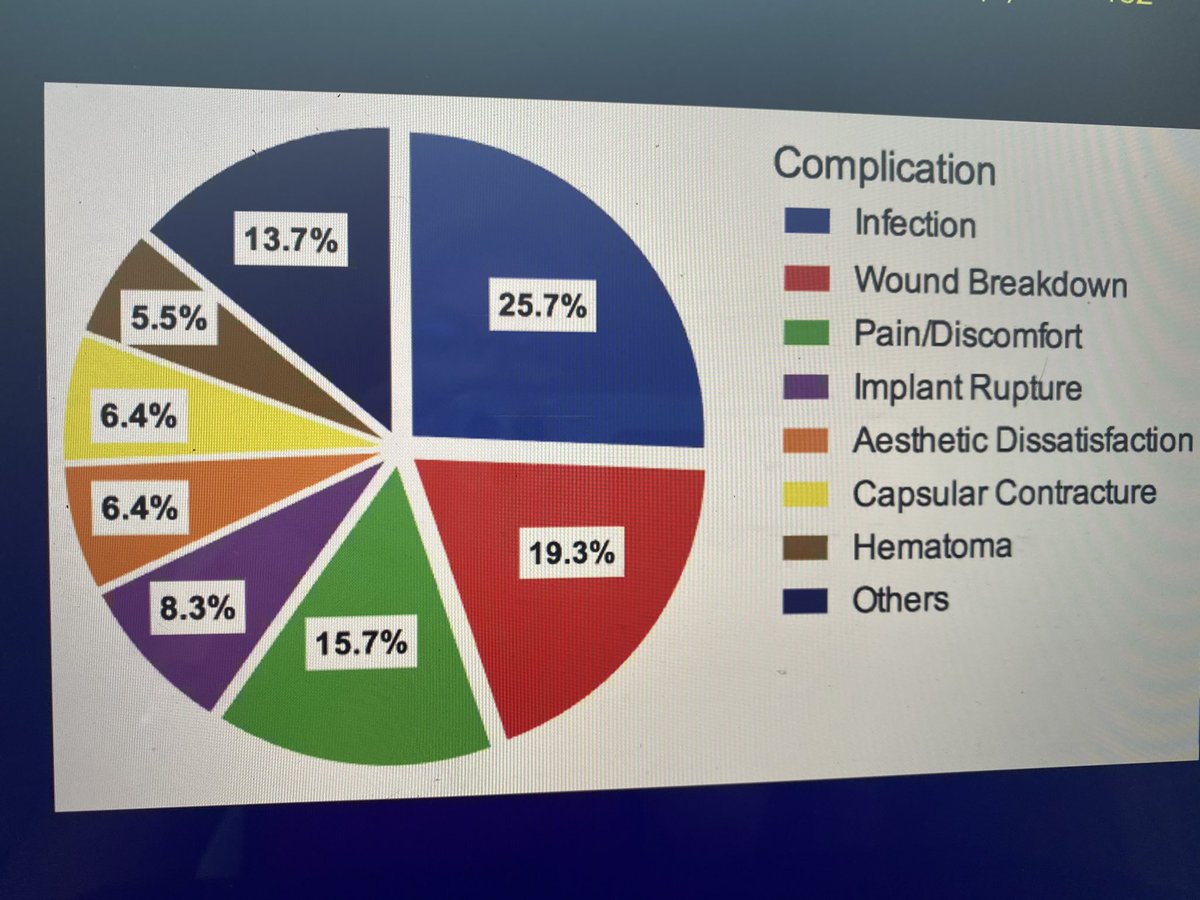
Kicking of the webinar with a presentation by Titus Adams Consultant Plastic Surgeon with a fabulous presentation emphasising the importance of post operative care and dangers of the cheapest possible price approach and aggressive online marketing #PEOPILwebinar
Important complications such as wound infection, breakdown and pain often present as late complications following surgery. Access to the surgeon or clinic may be difficult. Access to notes Lack of follow up. Communication issues. Lack of data 
Handing over to Isabel Bathurst, Solicitor Advocate from Scott-Moncrieff and Associates highlighting the cases of surgery abroad where people have died following cheap procedures. The cost of revision is over 30 billion over last 5 years. 
Last speaker Babs Forman of Skin Confident Ltd. Speaking on the use of skin camouflage to try and help people to deal with the psychological aspects of scarring and skin damage. Consideration should be given to including costs in claims for clients.
• • •
Missing some Tweet in this thread? You can try to
force a refresh