Excellent paediatric transfusion session @AABB #AABB2020
First Megan Delaney discussing the role of pathogen inactivation in platelets transfused to children and neonates.
First Megan Delaney discussing the role of pathogen inactivation in platelets transfused to children and neonates.
Updating on the recent evidence supporting the safety of both Mirasol and Intercept products, but highlighting that both result in lower post transfusion platelet increments.
Then Marianne Nellis @mnellismd talking on transfusion in paediatric critical care, presenting the work of the TAXI (Transfusion and Anaemia eXpertise Initiative group), culminating in a series of best practice statements and a transfusion decision tree.
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…

Following on from this will be TAXI-CAB (Control/Avoidance of Bleeding) – aiming for publication early next year. Amazing work!
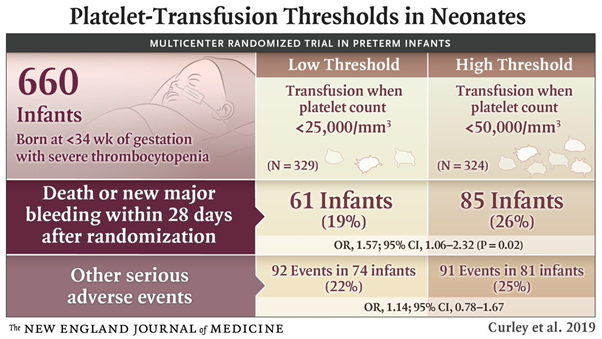
Then @simonstanworth on the PlaNeT-2 study. Neonates were randomised to receiving platelets at 25 or 50 x10^9/L. Full study was published last year nejm.org/doi/10.1056/NE…
Paediatric practice has historically been to use more liberal thresholds in neonates versus adults (where 10 would be our standard in stable patients). @BritSocHaem guidelines state 25 for stable neonates.
onlinelibrary.wiley.com/doi/full/10.11…
onlinelibrary.wiley.com/doi/full/10.11…

Bleeding/death composite outcome occurred in 19% in the restrictive group and 26% in the liberal group. OR 1.57 (1.06-2.32) i.e. outcomes worse in the patients receiving platelets at 50.
This was unexpected. Differences materialised from the second week after randomisation.
This was unexpected. Differences materialised from the second week after randomisation.
Why is this? Volume? Platelet donors are adults; are there physiological differences between adult and neonatal platelets and plasma? Is there an immune/inflammatory effect?
Other studies are also reporting worsening outcomes with platelet transfusion and a threshold of 25 is now recommended for neonatal platelet transfusions
ashpublications.org/blood/article-…
ashpublications.org/blood/article-…
Thanks for a great session!
• • •
Missing some Tweet in this thread? You can try to
force a refresh




