Sir Mansel Aylward talks about his experience of #LongCovid
bbc.co.uk/news/uk-wales-…
bbc.co.uk/news/uk-wales-…
I hope his reflections go slightly deeper than just the UK's unpreparedness... meassociation.org.uk/2011/11/privat…
Further reading from @TommyShakes | Blaming the victim, all over again: Waddell and Aylward's biopsychosocial (BPS) model of disability
journals.sagepub.com/doi/abs/10.117…
journals.sagepub.com/doi/abs/10.117…
More further reading: Getting rich on disability denial @RedPeppermag redpepper.org.uk/getting-rich-o…
Psychological tyranny prescribed by the DWP: preventable harm is government policy | B J Gen Pract 2018
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…
Who is Prof Sir Mansel Aylward? lshubwales.com/board/professo…
Problems in the assessment of psychosomatic conditions in Social Security benefits and related commercial schemes | J Psychosom Res 1995 pubmed.ncbi.nlm.nih.gov/8568732/
Models of sickness and disability | Waddell and Aylward 2010 webility.md/praxis/downloa…
Who was Gordon Waddell journals.lww.com/pain/Citation/…
When actually this seems to be a description of one of a number of different scenarios, where the ideal "model" is at the top. 

From my own experience, application of BPS in healthcare, rather than addressing complex issues in a multifactorial way, essentially reduces it to "guided self-help", and further exacerbates the problem.
Dog whistle medicine and disability denial - Unum, Aylward and the "Wessely School"
https://x.com/newhealthpsych/status/1375085863818952708
Aylward also contributed a section to the Trends in Health and Disability 2002 report (Unum) - it's quite dry though. The section by a certain Dr Sharpe is more interesting... web.archive.org/web/2003012615…
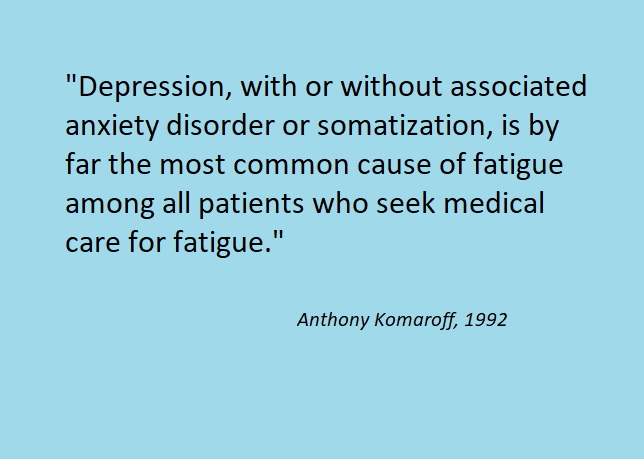
"Both State and private insurers pay people to remain ill."
Nice dig at patient support groups and charities there too. 😠
Nice dig at patient support groups and charities there too. 😠

Sharpe mentions the 2002 CMO report, which I linked to here:
https://x.com/_Lucibee/status/1372869367512363012
"Neither classification [DSM-IV vs ICD-10] is ideal."
aka "We're not saying that it's psychological... (but it's psychological.)"
aka "We're not saying that it's psychological... (but it's psychological.)"

"The trial was co-designed with a patient group."

https://x.com/zaranosaur/status/1376219252810735622

Another clipping to append to this thread...
https://x.com/maxwhd/status/1378406787498582017
@threadreaderapp please unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh