1/ I often get asked about the presence of granular casts on the automated UA reported by the lab whether it is equivalent to seeing muddy brown casts.
❓Do you think granular casts can be used to diagnose ATN?
More to see in #NephMadness on #liquidbiopsy
@NSMCInternship
❓Do you think granular casts can be used to diagnose ATN?
More to see in #NephMadness on #liquidbiopsy
@NSMCInternship
2/ Spin the urine! This is one of the maneuvers that I enjoy doing with residents the most as there is a lot to uncover.
I totally underestimated the power of this test. How many times have you spun the urine yourself before nephrology training?
I totally underestimated the power of this test. How many times have you spun the urine yourself before nephrology training?
3/ The clinical properties of urine have long been described by the medical community.
‘Diabetic’ (polyuric) disorders were classified as ‘mellitus’ (honey-sweet) or ‘insipidus (flavorless) based on the urine’s taste!
#NephMadness #liquidbiopsy
‘Diabetic’ (polyuric) disorders were classified as ‘mellitus’ (honey-sweet) or ‘insipidus (flavorless) based on the urine’s taste!
#NephMadness #liquidbiopsy

4/ Acute tubular necrosis (ATN) is the most common cause of AKI in hospitalized patients. I look for muddy brown casts and renal tubular cells.
An excellent RFN post by @VelezNephHepato clearly explains why we see these markers of ATN in the urine.
renalfellow.org/2019/04/30/uri…
An excellent RFN post by @VelezNephHepato clearly explains why we see these markers of ATN in the urine.
renalfellow.org/2019/04/30/uri…
5/ As with all test interpretation, it is best to start with assessing pre-test probabilities of disease.
For patients with high suspicion for ATN, I would be content with even a few muddy brown casts or renal tubular cells.
For patients with high suspicion for ATN, I would be content with even a few muddy brown casts or renal tubular cells.

6/ Renal tubular epithelial (RTE) cells are a little more tricky to identify. RTE resembles urothelial cells which are usually more cuboidal in nature and often in clumps.
See this blog by @swissnephro for wonderful detail
renalfellow.org/2020/07/13/uri…
See this blog by @swissnephro for wonderful detail
renalfellow.org/2020/07/13/uri…

7/ Why do you need urine sediment when you can diagnose clinically? How does confirming ATN alter management? Curious to hear your thoughts as well
I will name several benefits in the Tweets that follow and would love to hear more thoughts.
#AskRenal #SpinUrine #PisseProphets
I will name several benefits in the Tweets that follow and would love to hear more thoughts.
#AskRenal #SpinUrine #PisseProphets

8/ Benefit 1: Unabashed diuresis.
I am more confident in my recommendation to diurese a patient with hypervolemia aggressively when they have signs of ATN on microscopy comparatively to suspected ATN.
#SpinUrine #PisseProphets #NSMC #NephMadness
I am more confident in my recommendation to diurese a patient with hypervolemia aggressively when they have signs of ATN on microscopy comparatively to suspected ATN.
#SpinUrine #PisseProphets #NSMC #NephMadness
9/ Benefit 2: Reassurance when Cr continues to rise.
When creatinine rise, it often causes some panic and perhaps some decisions paralysis
If we knew it is ATN, it is easier just acknowledged the rise and move on to the next problem
When creatinine rise, it often causes some panic and perhaps some decisions paralysis
If we knew it is ATN, it is easier just acknowledged the rise and move on to the next problem
10/Benefit 3: Faster diagnosis.
Urine sediments precede the clinical upward trend of creatinine, hence preventing delayed diagnosis of AKI.
Yupp, AKI happens 2 days ago. Now creatinine is 2.1 mg/dL
Urine sediments precede the clinical upward trend of creatinine, hence preventing delayed diagnosis of AKI.
Yupp, AKI happens 2 days ago. Now creatinine is 2.1 mg/dL
11/Benefit 4: Accelerate work up.
The lack of granular casts with no indication in history for ATN, additional etiologies for AKI like GN, TMA should be aggressively looked into.
Lack of casts however does not rule out ATN.
The lack of granular casts with no indication in history for ATN, additional etiologies for AKI like GN, TMA should be aggressively looked into.
Lack of casts however does not rule out ATN.
12/Benefit 5: Severity assessment.
Wall-to-wall muddy brown cast ATN pose a worse clinical scenario than scattered presence of renal tubular epithelial cells. Check out this awesome article on scoring system that can be used:
cjasn.asnjournals.org/content/5/3/402
@scoca1 @KidneydrChirag
Wall-to-wall muddy brown cast ATN pose a worse clinical scenario than scattered presence of renal tubular epithelial cells. Check out this awesome article on scoring system that can be used:
cjasn.asnjournals.org/content/5/3/402
@scoca1 @KidneydrChirag

13/ Another urine sediment finding that gets everyone excited is the ‘dysmorphic RBC’. See the excellent explanation in #NephMadness Liquid Biopsy region on the different dysmorphism that can occur!
ajkdblog.org/2021/03/01/nep…
@DrFlashHeart @swissnephro
ajkdblog.org/2021/03/01/nep…
@DrFlashHeart @swissnephro
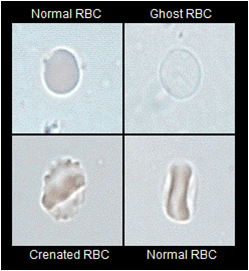
14/ I am still learning how to call differentiate RBC morphologies with accuracy. Many tools can assist with this, including phase contrast microscopy, peripheral blood smear analysis and urine osmolality/specific gravity.
#SpinUrine #PisseProphets @MGHKidneys @BWHKidney
#SpinUrine #PisseProphets @MGHKidneys @BWHKidney

15/ Phase contrast microscopy helps to enhance the edge of particles. In this picture, it is much easier to see the acanthocyte’s “Mickey Mouse ears” compared to bright field imaging. Hyaline casts are also much easier to spot.
#SpinUrine #PisseProphets
#SpinUrine #PisseProphets

16/ Is peripheral blood smear (PBS) important? Yes!
I had a patient with echinocyte in PBS. And I see them in the urine
Is it dysmorphic because of the glomerular process?
Or is it initially dysmorphic from the blood?
Turns out the patient has IgAN!
I had a patient with echinocyte in PBS. And I see them in the urine
Is it dysmorphic because of the glomerular process?
Or is it initially dysmorphic from the blood?
Turns out the patient has IgAN!
https://twitter.com/janewitwong/status/1347570219993034756?s=20
17/ Urine osmolality (and its UA cousin, specific gravity) can help contextualize RBC morphology.
High urine specific gravity can result in crenated RBC while low urine specific gravity may result in ghost cells.
High urine specific gravity can result in crenated RBC while low urine specific gravity may result in ghost cells.
18/ To learn more about the urine sediment, aka the liquid biopsy, enjoy the #NephMadness article on this.
ajkdblog.org/2021/03/01/nep…
Submit your favourite #SpinUrine for the contest this month!
Thank you @DrFlashHeart @docanjuyadav @amyaimei for this craft of tweetorial!
ajkdblog.org/2021/03/01/nep…
Submit your favourite #SpinUrine for the contest this month!
Thank you @DrFlashHeart @docanjuyadav @amyaimei for this craft of tweetorial!
Also thank you @iheartkidneys for topic selection @VelezNephHepato for all the inspiring tweets on sediments in the past and @NSMCInternship faculty for this first craft of tweetorial
• • •
Missing some Tweet in this thread? You can try to
force a refresh




