1/
1st week of NeuroICU fellowship. A #tweetorial summary:
1⃣ Pt in DI. Give anti-diuretic hormone (ADH), call it “pit drip”
2⃣Pt in distributive shock. Give ADH, call it “vaso”
3⃣Pt on ASA needs EVD. Give ADH (sort of), call it “DDAVP”
4⃣ Fellow postcall & confused, give….
1st week of NeuroICU fellowship. A #tweetorial summary:
1⃣ Pt in DI. Give anti-diuretic hormone (ADH), call it “pit drip”
2⃣Pt in distributive shock. Give ADH, call it “vaso”
3⃣Pt on ASA needs EVD. Give ADH (sort of), call it “DDAVP”
4⃣ Fellow postcall & confused, give….

3/
All the names and purposes of ADH had me feeling ⬇️
So – a review of all things ADH including:
✅It’s various aliases
✅Receptors and function
✅Clinical utility in NeuroICU (+general ICUs)
All the names and purposes of ADH had me feeling ⬇️
So – a review of all things ADH including:
✅It’s various aliases
✅Receptors and function
✅Clinical utility in NeuroICU (+general ICUs)
4/
Starting with nomenclature:
Anti-diuretic hormone, desmopressin, DDAVP, vasopressin, AVP, Pitressin, Vasostrict – are they really all the same?
Not quite.
Starting with nomenclature:
Anti-diuretic hormone, desmopressin, DDAVP, vasopressin, AVP, Pitressin, Vasostrict – are they really all the same?
Not quite.
5/
Anti-diuretic hormone (ADH) and arginine vasopressin (AVP) can be used interchangeably for the neurohypophyseal hormone secreted by the posterior pituitary.
Structure from
Vasopressin: a concise review pubmed.ncbi.nlm.nih.gov/16793628/
Anti-diuretic hormone (ADH) and arginine vasopressin (AVP) can be used interchangeably for the neurohypophyseal hormone secreted by the posterior pituitary.
Structure from
Vasopressin: a concise review pubmed.ncbi.nlm.nih.gov/16793628/

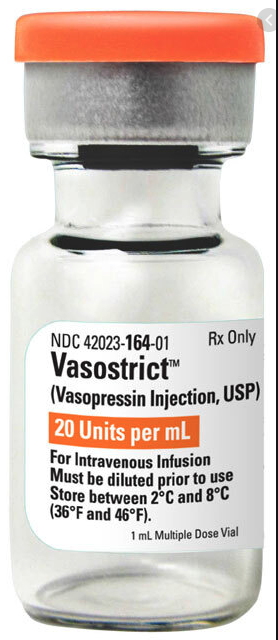
6/
Pitressin® (the “pit drip”) = trade name of a synthetic vasopressin solution. Can be made for IV, IM, SC or even intranasal
Vasostrict® = trade name for synthetic vasopressin solution, IV.
Both: 1mL = 20 units vasopressin.
Usually reconstituted in 50mL, thus 1mL = 0.4u

Pitressin® (the “pit drip”) = trade name of a synthetic vasopressin solution. Can be made for IV, IM, SC or even intranasal
Vasostrict® = trade name for synthetic vasopressin solution, IV.
Both: 1mL = 20 units vasopressin.
Usually reconstituted in 50mL, thus 1mL = 0.4u

7/
In contrast, desmopressin acetate is a synthetic analogue of ADH. The diff is there is a D-arginine for L-arginine @ pos. 8 & Pos.1 is deaminated.
DDAVP ® is a trade name.
Consequence of these structural tweaks = desmopressin ⬇️vasopressor action & ⬆️ antidiuretic action
In contrast, desmopressin acetate is a synthetic analogue of ADH. The diff is there is a D-arginine for L-arginine @ pos. 8 & Pos.1 is deaminated.
DDAVP ® is a trade name.
Consequence of these structural tweaks = desmopressin ⬇️vasopressor action & ⬆️ antidiuretic action
8/
Part 2: Function
How does ADH prevent diuresis?
Plasma omolarity (>280 mOsm), hypotension, and hypovolemia all trigger release of ADH. As can nausea, pain, and neuropathology (enter, SIADH...)
cvphysiology.com/Blood%20Pressu…
Part 2: Function
How does ADH prevent diuresis?
Plasma omolarity (>280 mOsm), hypotension, and hypovolemia all trigger release of ADH. As can nausea, pain, and neuropathology (enter, SIADH...)
cvphysiology.com/Blood%20Pressu…

9/
ADH then binds to *V2⃣ receptors* in the principal cells of the kidney collecting system.
Binding to V2⃣ receptors increases water and urea permeability = ⬆️water reabsorption.
Image: tinyurl.com/46yhekft
ADH then binds to *V2⃣ receptors* in the principal cells of the kidney collecting system.
Binding to V2⃣ receptors increases water and urea permeability = ⬆️water reabsorption.
Image: tinyurl.com/46yhekft

10/
You can remember that V2⃣ receptors increase H2⃣O retention.
AVP and DDAVP both bind here, but DDAVP has a much stronger affinity to these receptors.
You can remember that V2⃣ receptors increase H2⃣O retention.
AVP and DDAVP both bind here, but DDAVP has a much stronger affinity to these receptors.
11/
In the NeuroICU, we’re primarily using ADH in this context to treat central DI resulting from transsphenoidal adenomectomy (TSA) or cerebral herniation resulting compression of pit stalk/gland.
A vasopressin bolus and gtt are usually the initial choice for DI treatment.
In the NeuroICU, we’re primarily using ADH in this context to treat central DI resulting from transsphenoidal adenomectomy (TSA) or cerebral herniation resulting compression of pit stalk/gland.
A vasopressin bolus and gtt are usually the initial choice for DI treatment.
12/
We often given vasopressin 2.5-5unit IV while waiting for the gtt, and then give 0.25-1 unit/hour which is titrated to Uosm, UOP, and serum sodium.
All of which need to be very, very closely monitored!
We often given vasopressin 2.5-5unit IV while waiting for the gtt, and then give 0.25-1 unit/hour which is titrated to Uosm, UOP, and serum sodium.
All of which need to be very, very closely monitored!
13/
Long term, DI is managed with desmopressin (DDAVP) given PO, nasally, subQ or IV.
As a PO drug, its absorption can be unpredictable. Finding right dose requires some trial & a lot of monitoring.
Typical:
PO dose: 0.1mg qHS - 0.3mg TID.
IV doses: 1-2mcg qHS to BID
Long term, DI is managed with desmopressin (DDAVP) given PO, nasally, subQ or IV.
As a PO drug, its absorption can be unpredictable. Finding right dose requires some trial & a lot of monitoring.
Typical:
PO dose: 0.1mg qHS - 0.3mg TID.
IV doses: 1-2mcg qHS to BID
14/
Totally counterintuitively ADH can also regulate the correction of Na+ in chronically hypovolemic hyponatremic patients
If that seems incredibly ludicrious (…why would we give a patient with ⬇️sodium H2O retention drug??) read: tinyurl.com/5fydkkh7 from @ibookCC.
Totally counterintuitively ADH can also regulate the correction of Na+ in chronically hypovolemic hyponatremic patients
If that seems incredibly ludicrious (…why would we give a patient with ⬇️sodium H2O retention drug??) read: tinyurl.com/5fydkkh7 from @ibookCC.
15/
So… ADH can be used to treat hypernatremia in central DI and prevent overcorrection of sodium in chronic hypovolemic hyponatremia. Vasopressin or desmopressin work for these purposes.
So… ADH can be used to treat hypernatremia in central DI and prevent overcorrection of sodium in chronic hypovolemic hyponatremia. Vasopressin or desmopressin work for these purposes.
16/
How does ADH result in vasoconstriction?
This is mediated by binding of ADH to V1⃣ receptors located in smooth muscles which triggers catecholamine-independent vasoconstriction.
Image: tinyurl.com/46yhekft
How does ADH result in vasoconstriction?
This is mediated by binding of ADH to V1⃣ receptors located in smooth muscles which triggers catecholamine-independent vasoconstriction.
Image: tinyurl.com/46yhekft

17/
Doses here are fixed @ either vasopressin 0.03 or 0.04 units/min.
Remember, the DI dose is vasopressin 0.5-1 unit/*hour*
I remember thinking that they were orders of magnitude different, but because of the time denominator, the shock dose is actually ~2-5x larger
Doses here are fixed @ either vasopressin 0.03 or 0.04 units/min.
Remember, the DI dose is vasopressin 0.5-1 unit/*hour*
I remember thinking that they were orders of magnitude different, but because of the time denominator, the shock dose is actually ~2-5x larger

18/
Finally, both vasopressin and desmopressin/DDAVP have intrinsic platelet activating properties
DDAVP has the added effect of releasing von Willebrand factor & F VIII from endothelial cells.
Image reminding u of the importance of vWF (image @NEJM)
Finally, both vasopressin and desmopressin/DDAVP have intrinsic platelet activating properties
DDAVP has the added effect of releasing von Willebrand factor & F VIII from endothelial cells.
Image reminding u of the importance of vWF (image @NEJM)

19/
Since the 1970s desmopressin was used to prevent bleeding in pt w/ 🔽vWF
The bleeding dose is a 1x IV Desmopressin 0.3mcg/kg (~20-30mcg).
For comparison, the anti-diuretic dose is 1-3mcg IV. The hemostasis dose is thus x10 higher.
Effect is max @ ~30 mins. last 6-8hr
Since the 1970s desmopressin was used to prevent bleeding in pt w/ 🔽vWF
The bleeding dose is a 1x IV Desmopressin 0.3mcg/kg (~20-30mcg).
For comparison, the anti-diuretic dose is 1-3mcg IV. The hemostasis dose is thus x10 higher.
Effect is max @ ~30 mins. last 6-8hr
20/
In the neuroICU we very commonly see patients with ICH who were taking ASA. PATCH trial (Lancet 2016) demonstrated worse outcomes in patients who received platelet transfusion to “reverse” ASA’s effect.
Given DDAVPs' platelet activating effect, this a good alternative?
In the neuroICU we very commonly see patients with ICH who were taking ASA. PATCH trial (Lancet 2016) demonstrated worse outcomes in patients who received platelet transfusion to “reverse” ASA’s effect.
Given DDAVPs' platelet activating effect, this a good alternative?
21/
Maybe?
Retrospective Assessment of Desmopressin Effectiveness & Safety in Patients w Antiplatelet-Associated Intracra pubmed.ncbi.nlm.nih.gov/31567345/
Early Admin of Desmopressin and Platelet Transfusion for Reducing Hematoma Expansion in Patients With Acut… pubmed.ncbi.nlm.nih.gov/32304415/
Maybe?
Retrospective Assessment of Desmopressin Effectiveness & Safety in Patients w Antiplatelet-Associated Intracra pubmed.ncbi.nlm.nih.gov/31567345/
Early Admin of Desmopressin and Platelet Transfusion for Reducing Hematoma Expansion in Patients With Acut… pubmed.ncbi.nlm.nih.gov/32304415/
22/
We need an RCT. The DASH trial is currently underway to answer this question: ncbi.nlm.nih.gov/pmc/articles/P…
We need an RCT. The DASH trial is currently underway to answer this question: ncbi.nlm.nih.gov/pmc/articles/P…

23/
What comes up even more frequently is when a patient presents with IPH/IVH or SAH and is in need of a STAT EVD, but was on antiplatelet therapy.
Can DDAVP be used in those cases to transiently ⬆️ VWF and promote platelet adhesion to limit tract-related hemorrhage?
What comes up even more frequently is when a patient presents with IPH/IVH or SAH and is in need of a STAT EVD, but was on antiplatelet therapy.
Can DDAVP be used in those cases to transiently ⬆️ VWF and promote platelet adhesion to limit tract-related hemorrhage?
24/
The short answer is we don’t know, but for placing an EVD in a patient on anti-platelets this has become fairly standard in @emoryneurocrit
Curious about what others are doing? @namorrismd @aartisarwal @soojin_soojin @SamBSnider @alvindasMD
The short answer is we don’t know, but for placing an EVD in a patient on anti-platelets this has become fairly standard in @emoryneurocrit
Curious about what others are doing? @namorrismd @aartisarwal @soojin_soojin @SamBSnider @alvindasMD
25/
Summary:
⭐️ADH/AVP/Vaso/Vasopressin/Pitressin/Vasostrict = same (V1/V2 action)
⭐️Desmopressin/DDAVP = slightly modified synthetic analogue (V2 action).
⭐️Formulation+dose matter in determining the effect.
thought/alt uses? @Capt_Ammonia @nickmmark @DxRxEdu @AvrahamCooperMD
Summary:
⭐️ADH/AVP/Vaso/Vasopressin/Pitressin/Vasostrict = same (V1/V2 action)
⭐️Desmopressin/DDAVP = slightly modified synthetic analogue (V2 action).
⭐️Formulation+dose matter in determining the effect.
thought/alt uses? @Capt_Ammonia @nickmmark @DxRxEdu @AvrahamCooperMD
• • •
Missing some Tweet in this thread? You can try to
force a refresh












