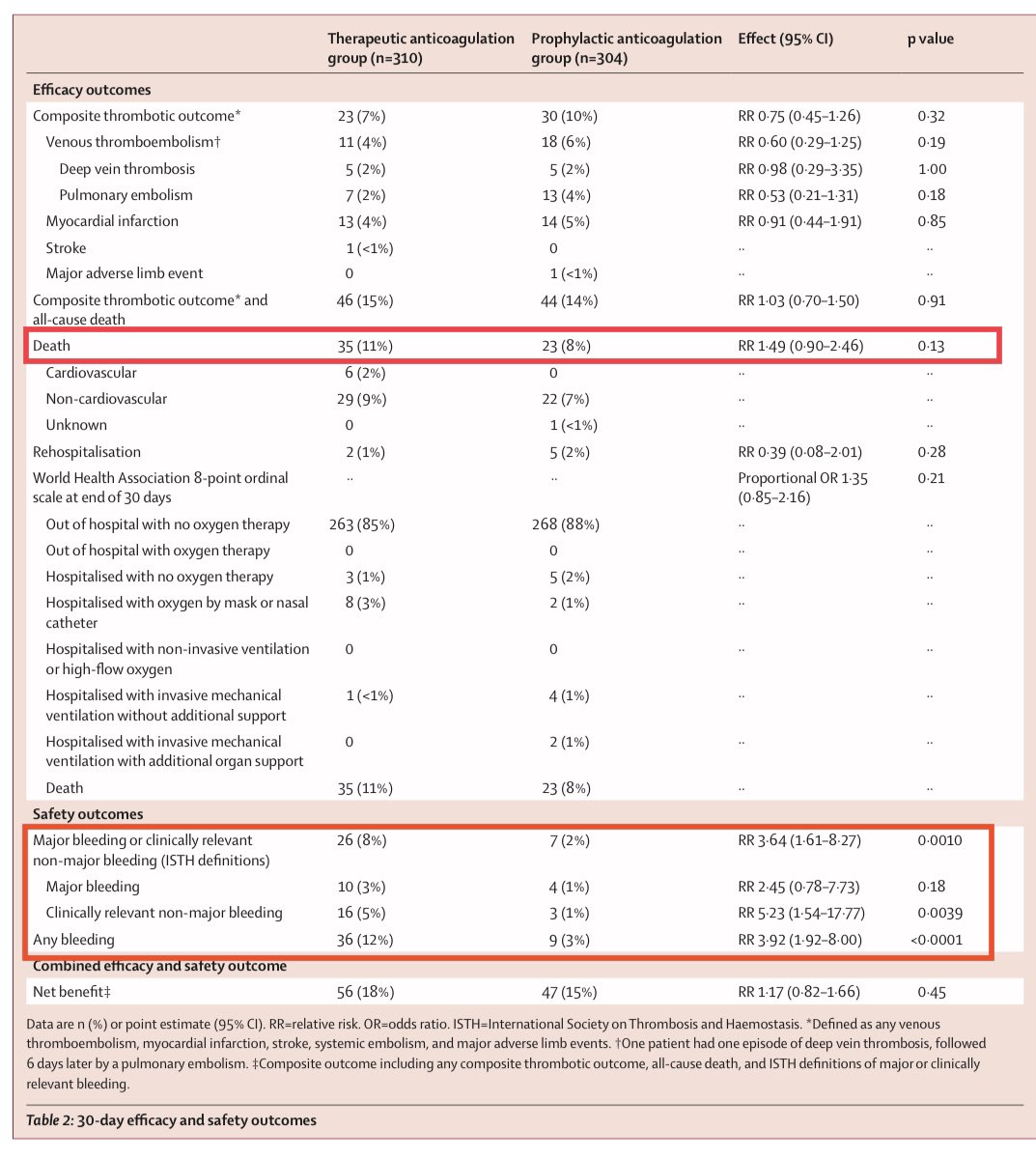
#ACTION RCT results just published @TheLancet: Another negative study of therapeutic #anticoagulantion (TA) in hospitalized people w/ COVID19:
- TA w/ rivaroxaban didn’t improve survival (or *any* endpoint) vs prophylaxis
- more bleeding with TA
1/
thelancet.com/journals/lance…



- TA w/ rivaroxaban didn’t improve survival (or *any* endpoint) vs prophylaxis
- more bleeding with TA
1/
thelancet.com/journals/lance…




The AntiCoagulaTlon cOroNavirus (ACTION) trial was a pragmatic open label RCT at 31 hospitals in 🇧🇷.
It enrolled hospitalized patients with COVID19 & an elevated D-dimer & randomized to TA vs prophylactic anticoagulation (PA).
Aside: not sure how I feel about that acronym...
2/
It enrolled hospitalized patients with COVID19 & an elevated D-dimer & randomized to TA vs prophylactic anticoagulation (PA).
Aside: not sure how I feel about that acronym...
2/

The intervention was TA with either a DOAC (rivaroxaban) if stable or LMWH (enoxaparin 1mg/kg BID) if unstable vs standard of care prophylaxis (UFH or LMWH).
Crossovers were allowed (eg if someone in the PA developed VTE). They adjusted dosing for renal function.
3/

Crossovers were allowed (eg if someone in the PA developed VTE). They adjusted dosing for renal function.
3/


The 1° endpoint was a hierarchical composite of time to death, duration of hospitalization, & duration of supplemental oxygen use up to day 30.
I’m always a little weary of composite endpoints that combine pt centered (survival) & non-pt centered endpoints (# of days on O2).
4/
I’m always a little weary of composite endpoints that combine pt centered (survival) & non-pt centered endpoints (# of days on O2).
4/
The groups were balanced & broadly representative of hospitalized COVID patients.
Most were stable (not in the ICU), on supplemental O2, w/o organ dysfunction. They don’t report APACHE or SOFA scores but overall not very sick at randomization. >80% received corticosteroids.
5/

Most were stable (not in the ICU), on supplemental O2, w/o organ dysfunction. They don’t report APACHE or SOFA scores but overall not very sick at randomization. >80% received corticosteroids.
5/


The 1° outcome was no different w/ TA & PA. There were more deaths, longer hospitalizations, & longer duration of O2. Plus a trend towards increased mortality with TA.
Both stable & unstable pts appeared to do WORSE with TA.
In fact, almost every subgroup did worse with TA.
6/



Both stable & unstable pts appeared to do WORSE with TA.
In fact, almost every subgroup did worse with TA.
6/



Statistical Aside: for those unfamiliar with “win ratio” don’t feel bad it’s a new method!
Win ratio is a method comparing multiple outcomes where there is a hierarchy of which outcome is most important (e.g deaths > readmissions)
Great explanation 👉academic.oup.com/eurheartj/arti…
7/



Win ratio is a method comparing multiple outcomes where there is a hierarchy of which outcome is most important (e.g deaths > readmissions)
Great explanation 👉academic.oup.com/eurheartj/arti…
7/




Specifically, the ACTION study found that therapeutic anticoagulation with DOACs was associated with numerically greater mortality (11% vs 8%). This wasn’t quite significant but the increase in major bleeding events was.
Overall a big 🚩for therapeutic anticoagulation.
8/
Overall a big 🚩for therapeutic anticoagulation.
8/

What does this add to our knowledge about AC in COVID?
-TH doesn’t improve outcomes in ICU pts (#REMAP)
-intermediate dose anticoag doesn’t help in ICU pts (#INSPIRATION)
-effect of TH in non-ICU pts unclear. REMAP suggests small benefit. #ACTION suggests no benefit/maybe harm
9/
-TH doesn’t improve outcomes in ICU pts (#REMAP)
-intermediate dose anticoag doesn’t help in ICU pts (#INSPIRATION)
-effect of TH in non-ICU pts unclear. REMAP suggests small benefit. #ACTION suggests no benefit/maybe harm
9/
One criticism is that DOACs may be different than LMWH in some crucial respects.
Plausible. Though DOACs are equivalent or better in most cases (afib, VTE, cancer, etc)
Also the “severe” patients who were treated with LMWH instead of DOSC didn’t do any better in survival
10/

Plausible. Though DOACs are equivalent or better in most cases (afib, VTE, cancer, etc)
Also the “severe” patients who were treated with LMWH instead of DOSC didn’t do any better in survival
10/


A recurring theme in COVID anticoag studies is that while many pts *develop* clots, few *die from* clots
Prophylactic dose is pretty effective. Therapeutic is more effective but still imperfect; we do see clots on TH occasionally
Crucially, preventing clots ≠ saving lives
11/
Prophylactic dose is pretty effective. Therapeutic is more effective but still imperfect; we do see clots on TH occasionally
Crucially, preventing clots ≠ saving lives
11/
Clinical 🥡
-#ACTION found Therapeutic anticoagulation (TA) w/ rivaroxaban or LMWH is NOT associated w/ improved survival or other benefits in hospitalized pts w/ COVID19
-no role for empiric TA with DOACs & probably no role for empiric TA at all in COVID19; use ppx instead
12/12
-#ACTION found Therapeutic anticoagulation (TA) w/ rivaroxaban or LMWH is NOT associated w/ improved survival or other benefits in hospitalized pts w/ COVID19
-no role for empiric TA with DOACs & probably no role for empiric TA at all in COVID19; use ppx instead
12/12
• • •
Missing some Tweet in this thread? You can try to
force a refresh
































