Pearls from @GlassockJ 's terrific talk on recurrent glomerulonephritis in kidney allografts at #GlomCon:
1) Recurrence of primary FSGS is as high as 70% in allografts (when genetic and secondary causes rigorously excluded) / 1
1) Recurrence of primary FSGS is as high as 70% in allografts (when genetic and secondary causes rigorously excluded) / 1
2) Recurrent FSGS in a second allograft when the first allograft was lost from recurrent FSGS is close to 100%, can be identified early by marked proteinuria /2
3) Risk factors for FSGS in allografts include Caucasian ancestry, young age, rapid course to ESKD, steroid resistance, low albumin, mesangial hypercellularity, and requirement for native nephrectomy /3
4) Potential/uncertain risk factors for recurrent FSGS: high urinary suPAR, permeability factor in vitro assay positive, anti-CD40 antibodies / 4
5) Treating with plasmapheresis early (within 30 days of recurrence) results in an improved response rate. Starting plasmapheresis 42+ days after recurrence, there is a very poor response / 5
6) Consider pre-emptive PLEX in FSGS patients at high risk of recurrence (no RCT results available though) / 6
7) IgA nephropathy recurs 30-40% in allografts by 5-10 years. Steroid-free immunosuppression increases the risk of recurrence. / 7
8) Predictors of increased risk of recurrence of IgA nephropathy - crescentic disease or IgA vasculitis, 2nd allograft with first lost from IgA N, lack of ATG induction, IL-10 polymorphisms, lanthanic IgA deposits in donor kidney, HLA identical grafts. / 8
9) 13.2% of allografts have donor-derived IgA deposits. Without time 0 biopsies and known cause of ESKD, can be mis-called recurrent IgA N, instead of donor-derived disease. /9
10) Primary MN recurs in 25-42% of allografts. Presence of PLA2R Abs in serum pre-transplant increase recurrence risk. /10
11) HLA-D (HAL-DRB1/HLA0DQA1) and PLA2R1 SNPs in the donor organ may increase risk of recurrence of MN. The genetic contribution of both the donor and recipient contribute to risk of recurrent MN in allografts. /11
12) Rituximab can induce remission, and for non-responders, various modalities are tried (but need more data) - robust anti-CD20 depletion (ofatumumab, obinutuzumab), cyclophosphamide, PLEX, MMF, cyclophosphamide, daratumumab (anti-CD38), and proteasome inhibitors. /12
13) Dense deposit disease has a high rate of recurrence in allografts (reported range of 20-100%). Highest risk is in patients with crescentic disease and complement factor H (CFH) mutations. Recurrence usually occurs in the first year. /13
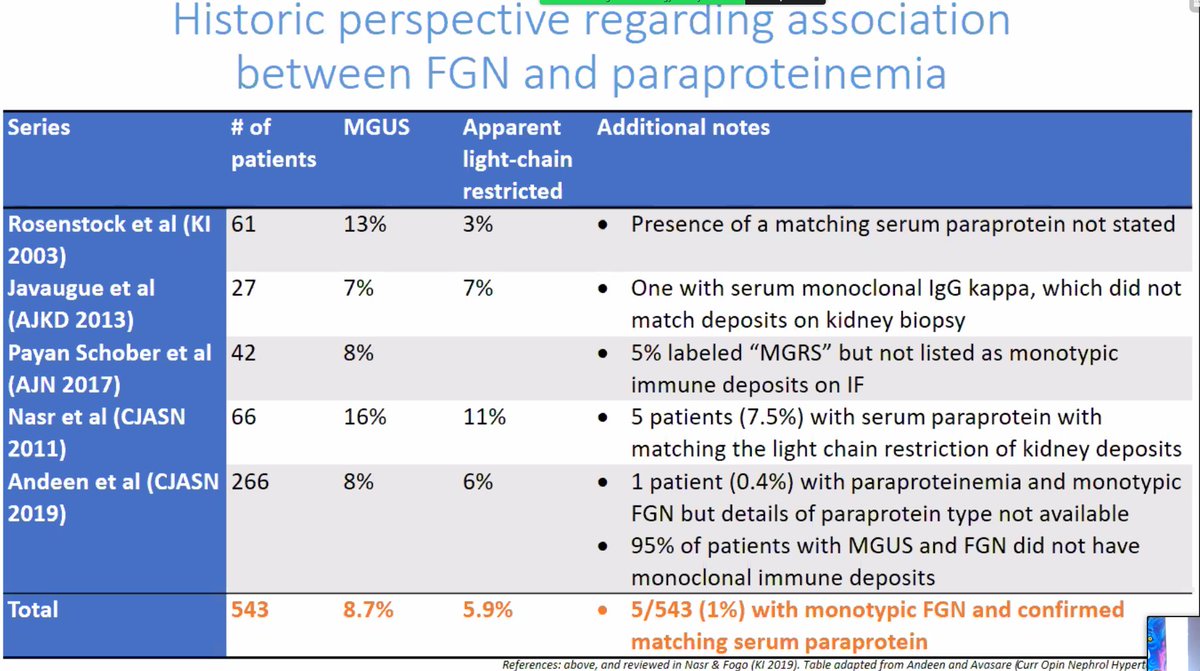
14) Fibrillary GN recurs in ~10-20% of allografts, recurrence is late (mean 5.7 years) / 14
15) Glomerular disease as the etiology of ESKD should not be considered a contraindication for transplantation, but careful monitoring and possibly protocol biopsies can allow for early identification of disease recurrence. /15
• • •
Missing some Tweet in this thread? You can try to
force a refresh