Our new report on medical staffing in England is out today. Nobody working in the NHS will be surprised to hear there are severe medical shortages in England. But the figures in our report show just how serious the situation is. THREAD bma.org.uk/staffing
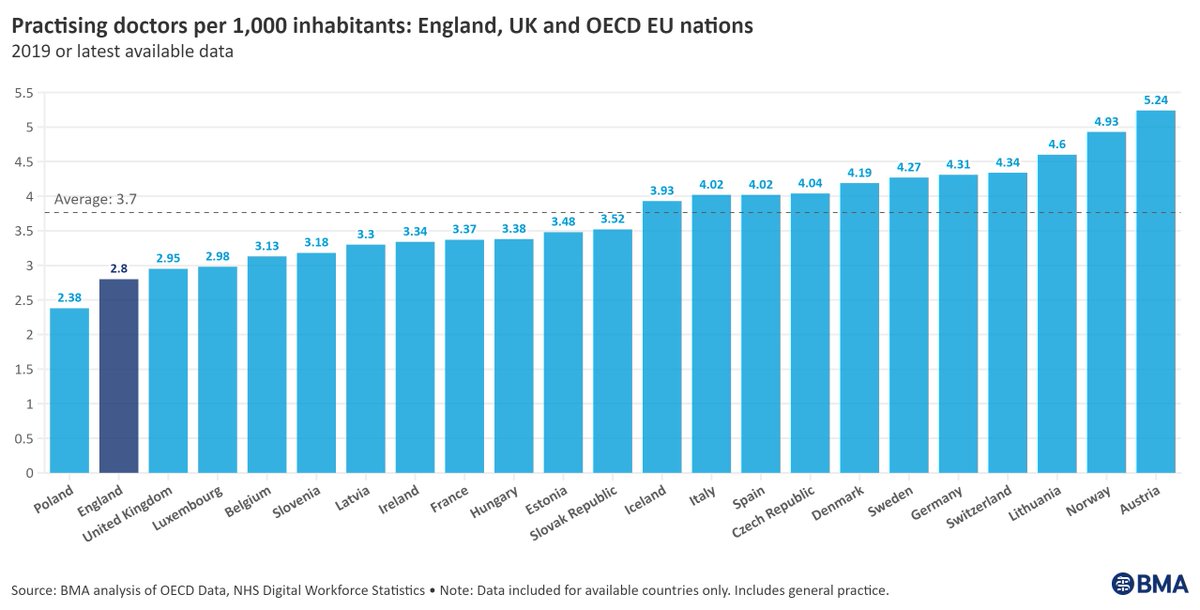
We need more doctors. There are currently 2.8 doctors per 1,000 people in England, while the average in comparable OECD EU countries is 3.7. Not a single region in England meets this ratio. 
If medical workforce growth remains at its current rate, it’ll be 2046 before the NHS has the number of practising doctors needed to raise our doctor/population ratio to 3.7.
That puts us 25 years behind our European neighbours.
That puts us 25 years behind our European neighbours.
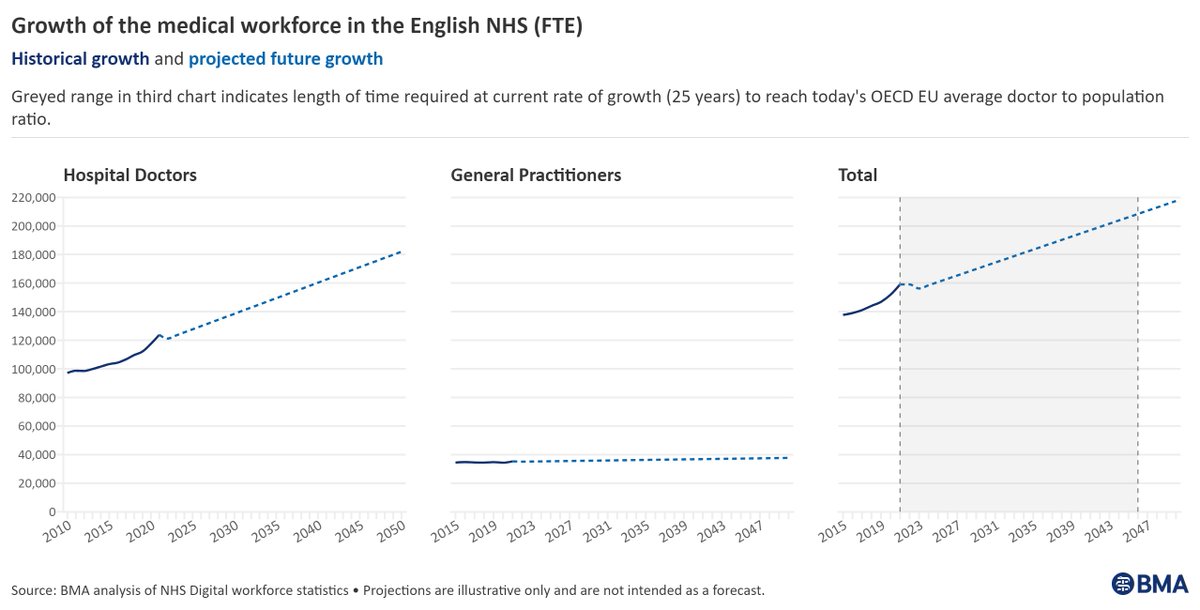
We estimate a current shortage of around 49,000 FTE (full-time equivalent) doctors and doctors in training in England across primary and secondary care.
These shortages mean that, on average, each FTE doctor in the NHS currently does 1.3 roles.
These shortages mean that, on average, each FTE doctor in the NHS currently does 1.3 roles.

The future doesn’t look better. Patient need is rising and by 2043, 1 in 4 of us will be over 65. Yet without significant intervention, we estimate the future medical workforce shortage to be between 27,000 and 84,000 full-time equivalent doctors.
We can do better.
We can do better.

Doctors are overworked and burnt out. Mounting evidence tells us that when doctors are working under conditions of chronic stress, mistakes are more likely to happen and moral injury and distress occur.
It doesn’t have to be this way.
It doesn’t have to be this way.

With the gap between doctor supply and patient need widening every year, necessary investment in the medical workforce can no longer be justifiably put off by our politicians.
To protect the future of doctors, patients, and our NHS, the Government must act today.
To protect the future of doctors, patients, and our NHS, the Government must act today.
The BMA is calling for:
- Primary legislation mandating regular healthcare workforce assessments in the Health and Care Bill
- Increased Treasury investment in the medical workforce, including expansion of medical school, foundation and specialty training places
- Primary legislation mandating regular healthcare workforce assessments in the Health and Care Bill
- Increased Treasury investment in the medical workforce, including expansion of medical school, foundation and specialty training places
To find out more, and to read our full call to action, read our full report: bma.org.uk/staffing 

• • •
Missing some Tweet in this thread? You can try to
force a refresh







