🧂 Hyponatremia #CaseReport #Tweetorial
(and a gif for the people who want to rename this hyperhydronemia)
(and a gif for the people who want to rename this hyperhydronemia)
Patient came to the hospital with abdominal pain, nausea, and vomiting. Patient has alcohol use disorder. Last drink was about a day prior to admission.
After arrival to the ER the patient has a seizure.
After arrival to the ER the patient has a seizure.
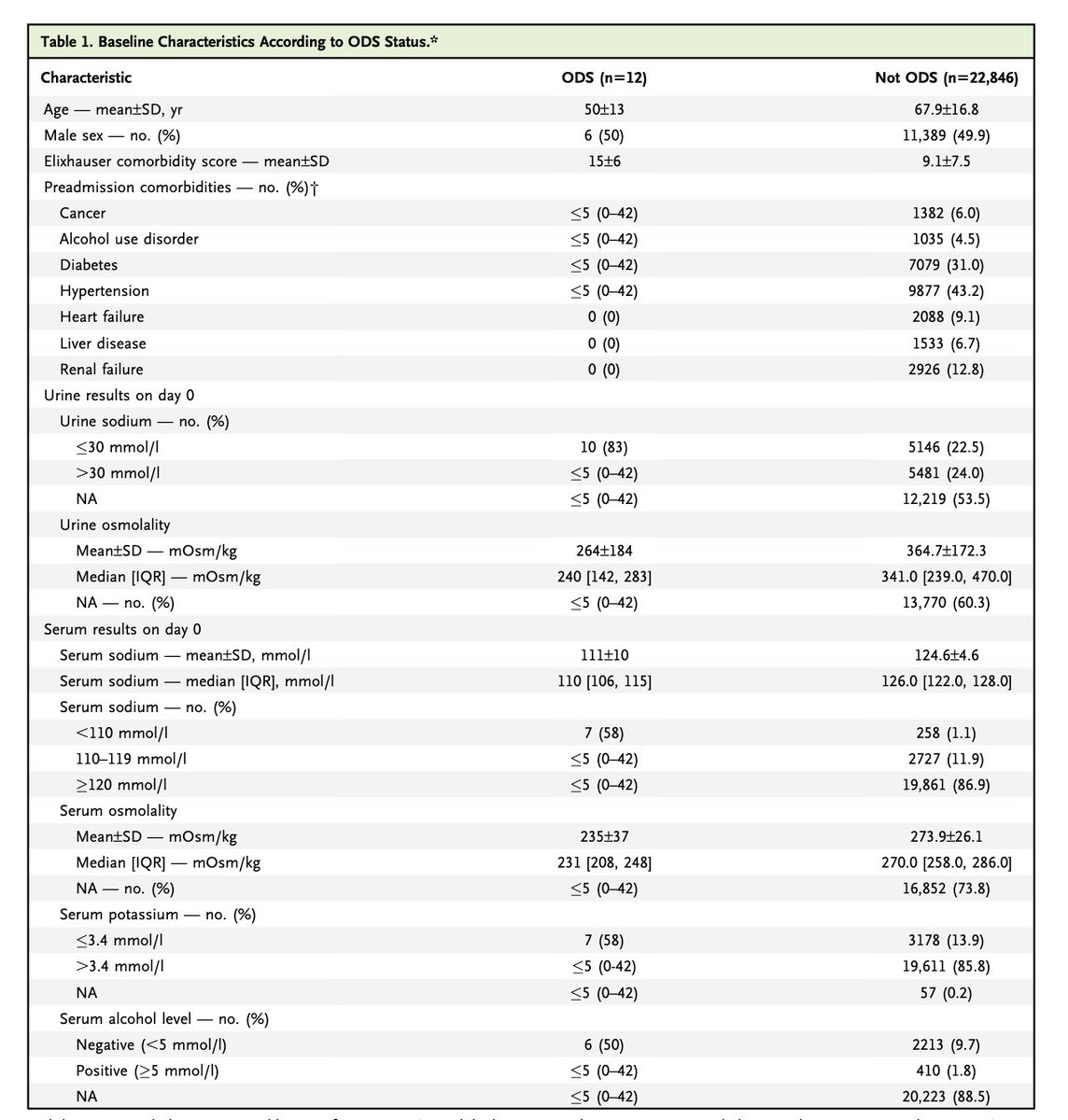
Besides the weirdly elevated anion gap, and the hypokalemia, the initial labs just show some AKI. I don't have an ABG but I suspect combined metabolic alkalosis and lactic acidosis. 

This can be demonstrated by looking at the Delta Ratio which compares the change in bicarb to the change in anion gap. The ratio should be 1. If it is less than 1, there is an additional non-anion gap metabolic acidosis, > 2 additional metabolic alkalosis 
A delta ratio of 6 is crazy high.
A related calculation, called the "bicarb before" can tell you the serum bicarb without the anion gap acidosis, so if the patient has two disorders it allows you to look at the metabolic alkalosis (or non-anion gap metabolic acidosis) without the anion gap metabolic acidosis. 

The "bicarb before" comes to a mostly unbelieable serum bicarb of 60.
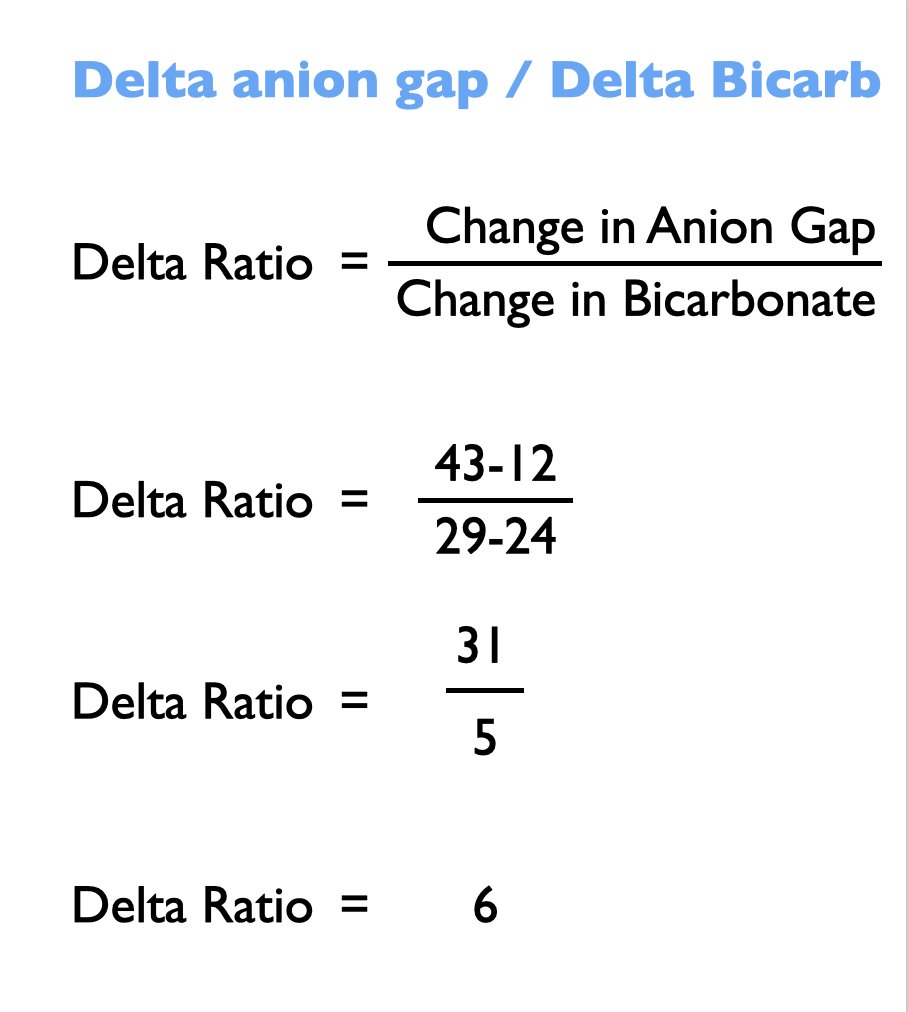
But the reason I was intrigued by the case are the next two labs that come 10 and 20 hours after the initial labs...The sodium drops to 125 despite getting 150 an hour of 0.9% NS and the patient making 3600 ml of urine. 



Additionally the full force of the metbolic alkalosis is revealed with the bicarb shooting from 29 to 41. I suspect this is due to vomiting. The urine chloride < 20 is consistent with this. This is Cl responsive metabolic alkalosis. It will (eventually) respond to the NS.
The urine also has a massive anion gap, around 90. What is the unmeasured anion?
(BTW the answer is bicarbonate)
But what is driving down the sodium? The patient appears volume depleted, and the steadily improving serum creatinine points to a patient with pre-renal AKI.
But what is driving down the sodium? The patient appears volume depleted, and the steadily improving serum creatinine points to a patient with pre-renal AKI.
In volume depletion hyponatremia, giving fluid improves the serum sodium, it doesn't make it worse. Also these patients do not typically make 3600 ml of urine
In it is highly unusual to make that much urine and have the sodium fall, usually that kind of urine output is associated with arising sodium. A hint to what is happenning can be found in the electrolyte free water clearance (Clefw). 
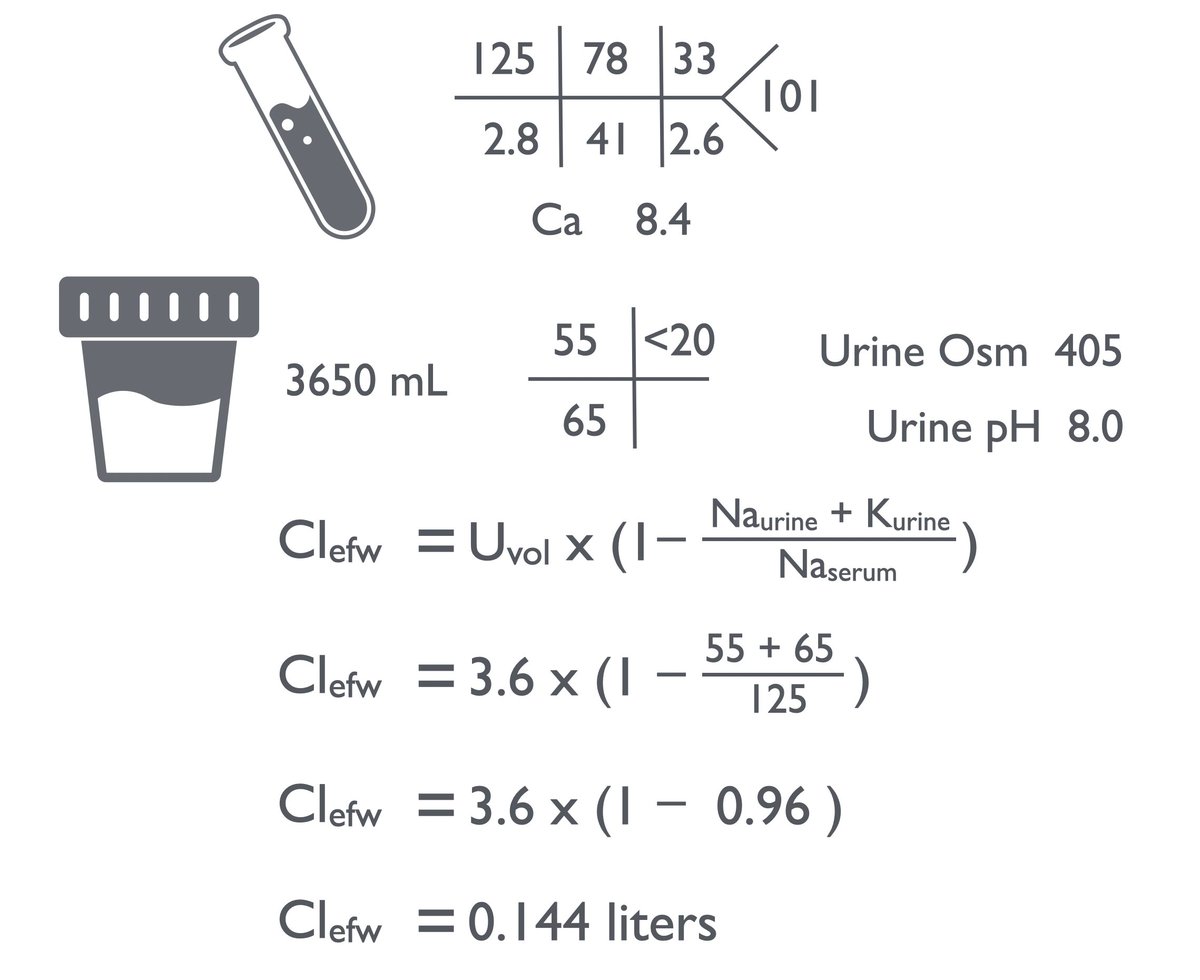
The high urine sodium and really high urine potassium makes the urine essentially isotonic to plasma. Even though the patient is making 3.6 liters, it is like taking ladles of soup from a big pot, no matter how many ladles you take out it doesn't change how salty the soup is.
Because the electrolyte free water is close to zero, those 3.6 liters of urine are not afffecting the serum sodium at all. So why is the sodium falling? I suspect this is due to the patient drinking (unrecorded) water.
So what would you do if faced with a falling sodium in a volume depleted patient?
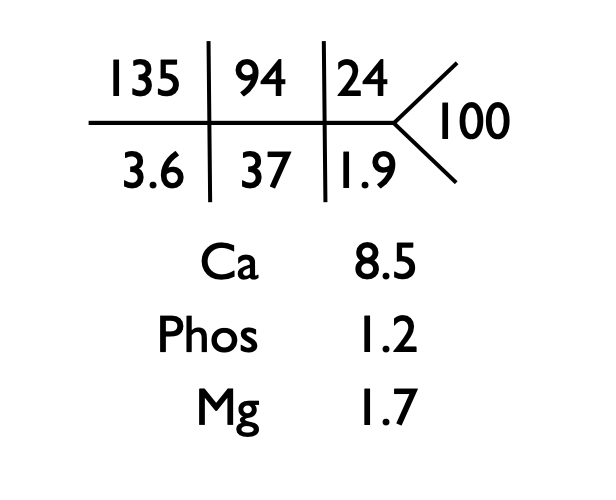
I chose Tolvaptan plus continued 0.9% NS at 150/hr. The following day, the labs look...better.
I think this patient had nausea induced ADH in addition to severe metabolic alkalosis and volume deficiency. I found it interesting.
I think this patient had nausea induced ADH in addition to severe metabolic alkalosis and volume deficiency. I found it interesting.
• • •
Missing some Tweet in this thread? You can try to
force a refresh