Soo NEJM has an educational COVID critical care “game.” Obviously I had to play on expert.
First off let’s talk about the name: Bagel Mage?!?
I’m not one to criticize - my name is just two synonymous verbs - but Bagel Mage 🥯 🧙♀️ sounds like the lamest D&D character ever.
1/

First off let’s talk about the name: Bagel Mage?!?
I’m not one to criticize - my name is just two synonymous verbs - but Bagel Mage 🥯 🧙♀️ sounds like the lamest D&D character ever.
1/


Bagel’s hypotensive with sats in the mid 80s, better do a quick assessment & start someO2.
“May I ask about your goals in the event of a cardiac or respiratory arrest?”
- maybe the worst possible way to ask this but here it goes…
…Ok I guess he’s an everything bagel.
2/
“May I ask about your goals in the event of a cardiac or respiratory arrest?”
- maybe the worst possible way to ask this but here it goes…
…Ok I guess he’s an everything bagel.
2/
No POCUS - guess I’ll do an exam & order some tests: ABG, basic labs, procalcitonin, CXR, some cultures, & a COVID test (you know “trust but verify”)
While I’m waiting I’ll order APAP, HFNC
Ugh oh. I guess im trouble for not coding enough. Damn this simulation is realistic!
3/
While I’m waiting I’ll order APAP, HFNC
Ugh oh. I guess im trouble for not coding enough. Damn this simulation is realistic!
3/

Ok - I entered some ICD9 codes to get that admin off my back.
Now they are all friendly (“your expert care is needed”) and I’m allowed get back to patient care.
Start some O2, order some Abx, and fire off a CXR & some labs…
4/
Now they are all friendly (“your expert care is needed”) and I’m allowed get back to patient care.
Start some O2, order some Abx, and fire off a CXR & some labs…
4/

Bad news: bilateral opacities on radiograph, he’s blowing off a lot of CO2 to protect oxygenation, and he’s COVID positive!
Better start some therapeutics. Ivermectin isn’t on formulary so I’ll stick to stuff that actually works: corticosteroids.
5/

Better start some therapeutics. Ivermectin isn’t on formulary so I’ll stick to stuff that actually works: corticosteroids.
5/


Ok I must have done something right: “Probability of a Good Outcome” just went from 0.00 to 0.36
Also, why is an anesthesiology ventilator just hanging out next to the bed in the ICU? Awkward.
6/

Also, why is an anesthesiology ventilator just hanging out next to the bed in the ICU? Awkward.
6/


No time to ponder the weird game artwork. This is getting serious!
“Doctor, Bagel Mage isn’t doing well”
7/
“Doctor, Bagel Mage isn’t doing well”
7/

More results back: 🧪 procal +, 🧫 growing staphylococcus aureus on blood cultures. Definitely no tocilizumab… good thing I already started Abx.
Getting nervous about that rising respiratory rate…
8/
Getting nervous about that rising respiratory rate…
8/

Uh oh I’m in trouble again - “a gentle and friendly reminder” in hospital admin parlance is serious!
I need to update my differential and do more documentation. Press Ganey scores are on the line!!!
10/
I need to update my differential and do more documentation. Press Ganey scores are on the line!!!
10/

Let’s reassess. We’ve tried HFNC, prone positioning, steroids, and antibiotics. Vitals and ABG look worse.
I ask a Bagel how he’s doing and he says “Bad”.
We could try NIPPV but I don’t think there is a quickly reversible cause here. Time to intubate.
11/

I ask a Bagel how he’s doing and he says “Bad”.
We could try NIPPV but I don’t think there is a quickly reversible cause here. Time to intubate.
11/


I tried hard to avoid intubation but ultimately it was necessary. Now Bagel is comfortably sedated on propofol and synchronous with the vent.
At least “Probability of a good outcome” is going up…
12/

At least “Probability of a good outcome” is going up…
12/


I guess his nurse doesn’t agree that he’s doing better.
“Have you considered…” consulting a better doctor? Ouch.
She’s right though. All hands on deck for Bagel. Let’s see what our esteemed consultants have to say…
13/
“Have you considered…” consulting a better doctor? Ouch.
She’s right though. All hands on deck for Bagel. Let’s see what our esteemed consultants have to say…
13/
Let’s try consulting pulm.
He’s just dying to tell me about the ARDSnet trial. That will make my next choice easier.
15/


He’s just dying to tell me about the ARDSnet trial. That will make my next choice easier.
15/



Sent a CRP, D-Dimer, & ferritin to keep my consultants happy. Perhaps a fecal occult blood test to go with that?
Clinically we’re stabilized: vented on LPV, Proned, on neuromuscular blockers (I don’t like to say “paralyzed” because it sounds scary to families), inhaled EPO
16/
Clinically we’re stabilized: vented on LPV, Proned, on neuromuscular blockers (I don’t like to say “paralyzed” because it sounds scary to families), inhaled EPO
16/

Speaking of stabilized - this game is super unstable running on Safari/iOS. It keeps reloading randomly.
I keep saving Bagel but then the game crashes and I have to start over…ugh
17/
I keep saving Bagel but then the game crashes and I have to start over…ugh
17/
The game keeps crashing & restarting. I should just do this in chrome but I’m too stubborn.
This causality loop is starting to make me go a little crazy & think insane “what if”thoughts. Should I use NS instead of LR? Dopamine instead of norepinephrine? (Like I said crazy😜)
18/
This causality loop is starting to make me go a little crazy & think insane “what if”thoughts. Should I use NS instead of LR? Dopamine instead of norepinephrine? (Like I said crazy😜)
18/
OK managed to get the game working properly in Chrome...
In fairness to NEJM, they do warn you about these stability issues in the directions.
The are also very clear that Bagel Mage is not based on any real life Bagels. They really don't want to get sued by a litigious 🥯
19/
In fairness to NEJM, they do warn you about these stability issues in the directions.
The are also very clear that Bagel Mage is not based on any real life Bagels. They really don't want to get sued by a litigious 🥯
19/

Anyway back to the case -
Bagel seems to be oxygenating better but I'm nervous about his hypotension. It would be great to have POCUS but i'll just cast a broad net...
Oh no. Bagel's troponin in 78 (nl <0.04) and his ECG doesn't look good!
20/
Bagel seems to be oxygenating better but I'm nervous about his hypotension. It would be great to have POCUS but i'll just cast a broad net...
Oh no. Bagel's troponin in 78 (nl <0.04) and his ECG doesn't look good!
20/

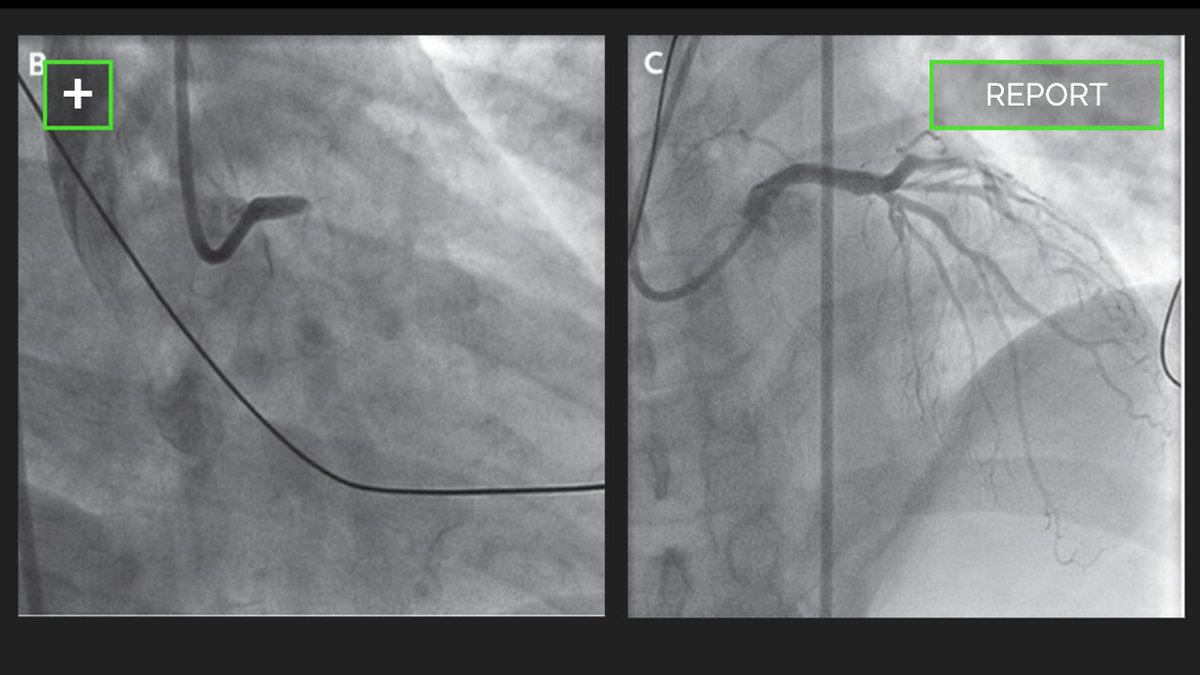
Looks like a STEMI: Time for ASA, a heparin gtt, STAT echo & an urgent call to (another) consultant: interventional cards!
This consultant is all business - no NEJM papers to read - she just PCI's the left main & drops the mic. The before after angiogram speaks for itself.
21/

This consultant is all business - no NEJM papers to read - she just PCI's the left main & drops the mic. The before after angiogram speaks for itself.
21/

Starting to feel good about this. Bagel is sick but the "probability of a good outcome" meter thinks he's gonna make it.
Hospital admin thinks so too & says "we could use another bed"
If STEMI+ARDS+COVID doesn't merit an ICU bed in this (fictional) universe, what does?
22/
Hospital admin thinks so too & says "we could use another bed"
If STEMI+ARDS+COVID doesn't merit an ICU bed in this (fictional) universe, what does?
22/

I guess my only choice in response to the hospital admin was "Got it!" (I must be on the fast track to promotion)
Now I get to make another high stakes decision:
- go to call room
- finish the shift
- start the day over again (another Groundhog day?)
Weird ending but OK...
23/
Now I get to make another high stakes decision:
- go to call room
- finish the shift
- start the day over again (another Groundhog day?)
Weird ending but OK...
23/

OK well that was interesting... this game was hokey but honestly it was also kinda enjoyable, in spite of all the crashes.
Hope you've enjoyed this weird rambling 🧵. If you want to save Bagel yourself, you can check out the NEJM site:
covid19rx.nejm.org/landing/index.…
24/24
Hope you've enjoyed this weird rambling 🧵. If you want to save Bagel yourself, you can check out the NEJM site:
covid19rx.nejm.org/landing/index.…
24/24
• • •
Missing some Tweet in this thread? You can try to
force a refresh