1/ Have you ever...
...promised yourself that THIS time you'll prioritize teaching while on the inpatient service but then get TOO BUSY?
...or WANT to teach something on rounds but realize that you have FORGOTTEN the details of that clinical pearl.
Then this week is for you!
...promised yourself that THIS time you'll prioritize teaching while on the inpatient service but then get TOO BUSY?
...or WANT to teach something on rounds but realize that you have FORGOTTEN the details of that clinical pearl.
Then this week is for you!
2/ This week, I will share tips to help you prepare to teach effectively on rounds as one of our “foundational skills” for inpatient teaching.
It's another #TweetorialTuesday from the @MedEdTwagTeam for our #MedTwitter & #MedEd friends.
It's another #TweetorialTuesday from the @MedEdTwagTeam for our #MedTwitter & #MedEd friends.

3/ Before we get started, I want you to reflect on something:
When you travel, do you tend to plan an itinerary for your trip or "wing it"?
Now, what if you only had a single day in that city but wanted to see all the famous sites?
Would your answer change?
When you travel, do you tend to plan an itinerary for your trip or "wing it"?
Now, what if you only had a single day in that city but wanted to see all the famous sites?
Would your answer change?

4/ I think teaching is very similar to traveling - you can either "wing it" or "plan it".
Both can be fun & effective.
BUT, you can teach MORE in LESS time if you plan your teaching.
Both can be fun & effective.
BUT, you can teach MORE in LESS time if you plan your teaching.

5/ So how do I prepare for teaching when I already have 10 million other things to do?
I select ONE thing to teach for each patient when I'm reviewing charts in the AM.
Doing this:
1. Ensures teaching HAPPENS.
2. Keeps my teaching FOCUSED.
3. ALIGNS teaching with patient care.
I select ONE thing to teach for each patient when I'm reviewing charts in the AM.
Doing this:
1. Ensures teaching HAPPENS.
2. Keeps my teaching FOCUSED.
3. ALIGNS teaching with patient care.

6/ This planning for teaching is WHY I believe in reviewing patients’ charts before rounds.
1⃣ It makes rounds more efficient since the team doesn't have to recite ALL data to me
2⃣ It allows me to quickly look up or review information prior to teaching if I need a refresher
1⃣ It makes rounds more efficient since the team doesn't have to recite ALL data to me
2⃣ It allows me to quickly look up or review information prior to teaching if I need a refresher

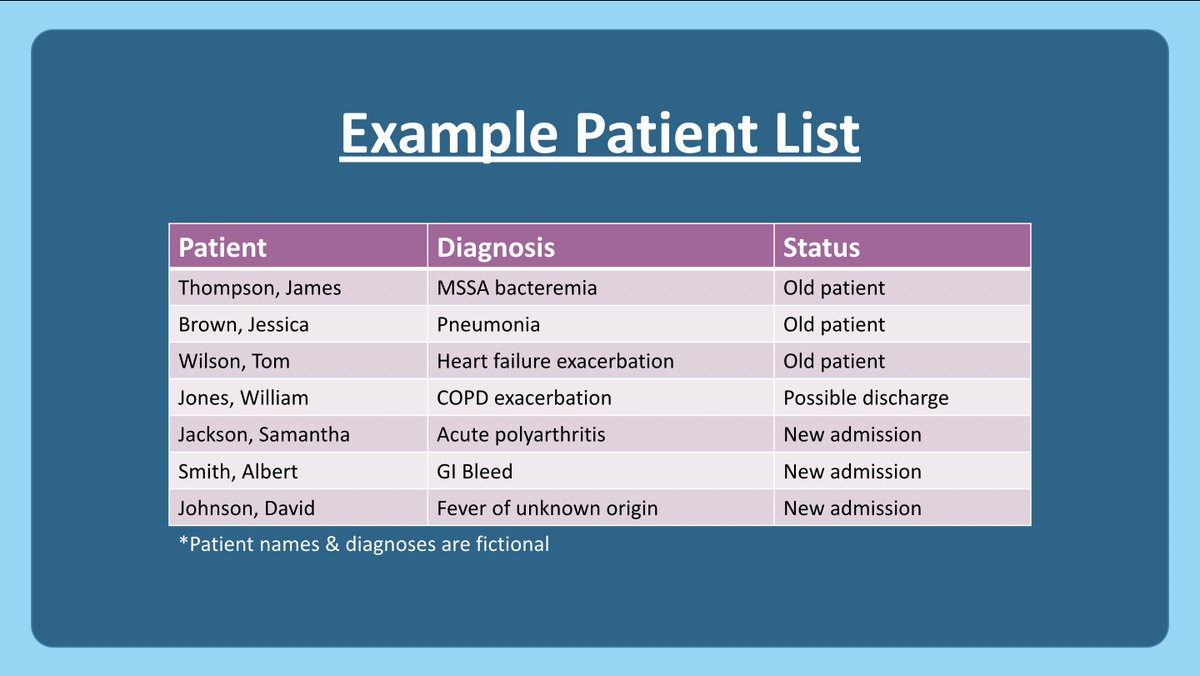
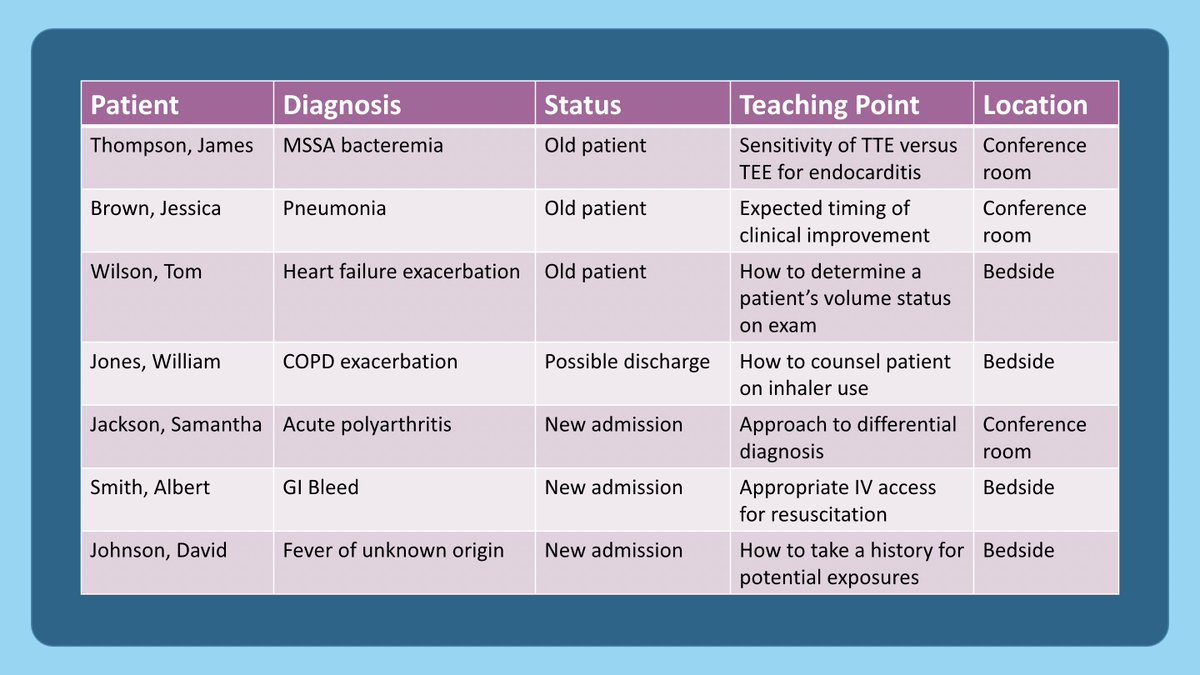
7/ So let's use this patient list to illustrate my process.
First, I consider WHAT content I want to teach.
Ideally, I try to teach something that I ALREADY KNOW or MUST look up to advance that patient's care. This avoids giving myself more prep work!
First, I consider WHAT content I want to teach.
Ideally, I try to teach something that I ALREADY KNOW or MUST look up to advance that patient's care. This avoids giving myself more prep work!
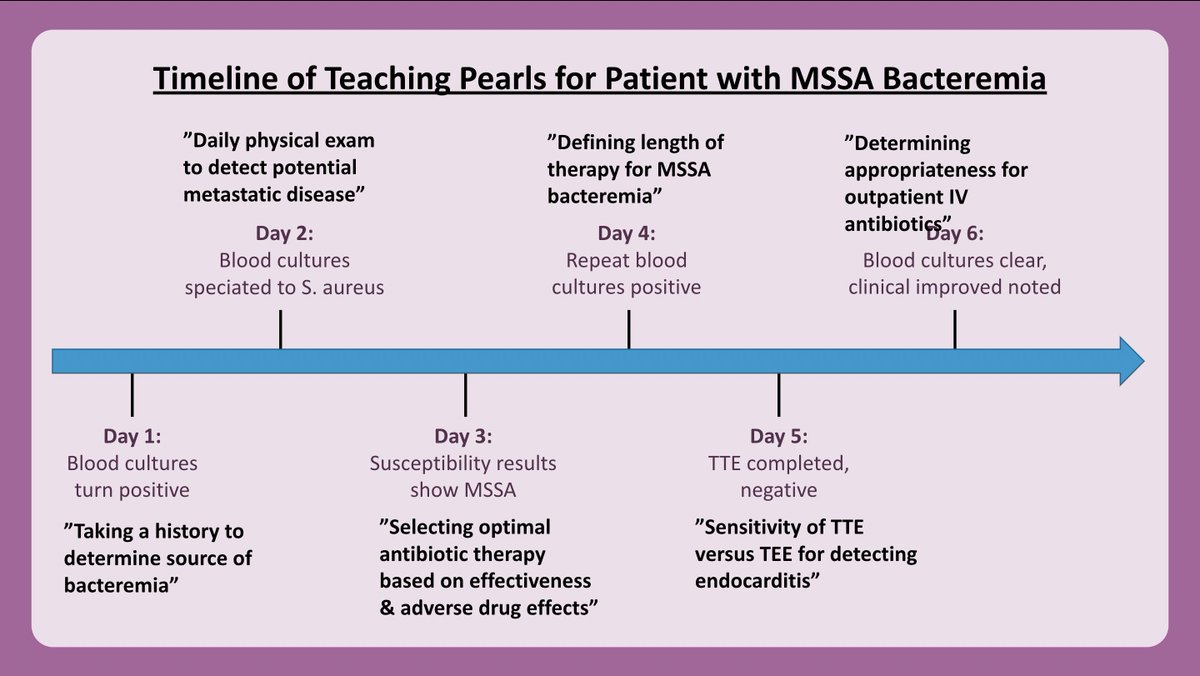
8/ Here are examples of teaching points that I was able to come up with from memory for the patient w/ MSSA bacteremia.
Although I may need to reference a few details (e.g., exact numbers for sensitivity of TTE), I can easily teach this content b/c this is a COMMON diagnosis.
Although I may need to reference a few details (e.g., exact numbers for sensitivity of TTE), I can easily teach this content b/c this is a COMMON diagnosis.

9/ New senior residents often tell me they fear they don't know enough to teach & feel they need to put in hours of preparation for teaching.
However, I bet all of us can easily come up w/ 1+ teaching point for every patient!
The challenge is LIMITING the teaching to ONE point.
However, I bet all of us can easily come up w/ 1+ teaching point for every patient!
The challenge is LIMITING the teaching to ONE point.
10/ Once you've come up with a list of potential teaching points, how do you decide which one to teach?
Well, I try to remember that I need a teaching point for EACH DAY of a patient's admission. Thus, I try to align my teaching with relevant patient care activities/decisions.
Well, I try to remember that I need a teaching point for EACH DAY of a patient's admission. Thus, I try to align my teaching with relevant patient care activities/decisions.

11/ Here's an example of how I may align my MSSA bacteremia teaching points with a patient's clinical course. 
12/ Once you have decided WHAT you want to teach, consider HOW & WHERE you want to teach it.
Some teaching points are better for the conference room where you have a white board to draw on (eg. developing a Ddx) whereas others are best at the bedside (eg. patient counseling).
Some teaching points are better for the conference room where you have a white board to draw on (eg. developing a Ddx) whereas others are best at the bedside (eg. patient counseling).
13/ New admissions or possible discharges often lend themselves best to teaching points at the bedside (yellow highlighter), although sometimes my teaching points fit better in the conference room where we have time & space to discuss our clinical reasoning (blue highlighter). 
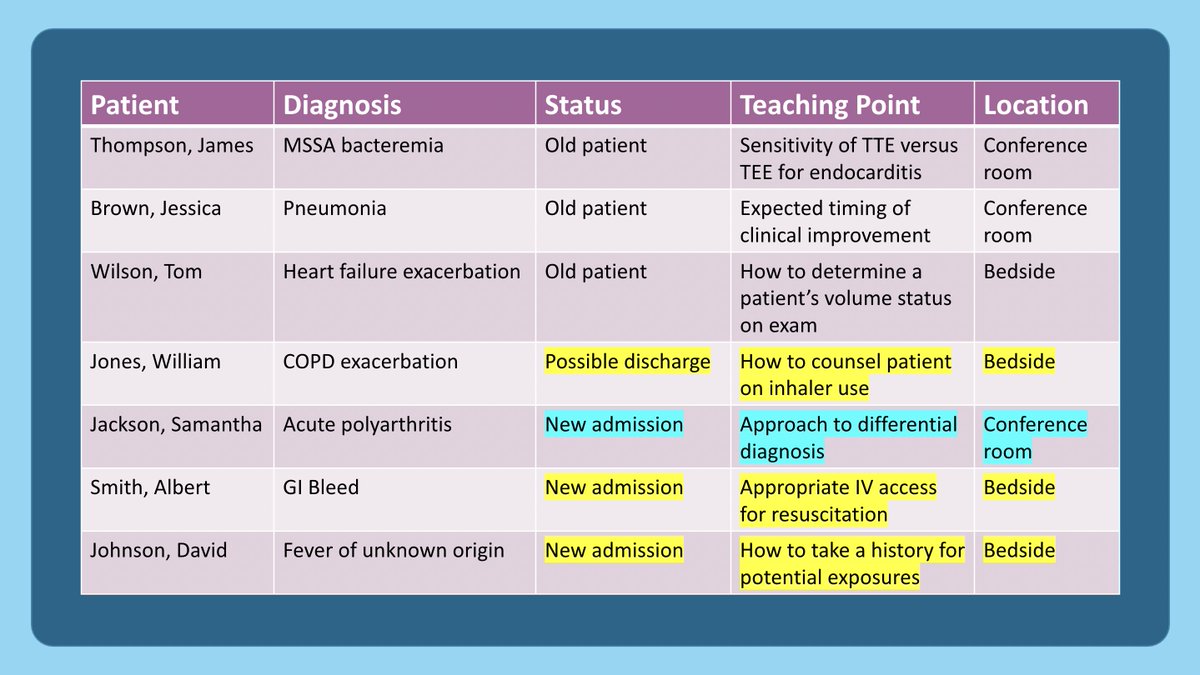
14/ Finally, I try to ensure that I'm diversifying my teaching by "mixing it up."
I try to ensure that I go beyond medical knowledge & patient care topics to actually teach the other ACGME competencies too!
For example, discussing ethical dilemmas can teach professionalism.
I try to ensure that I go beyond medical knowledge & patient care topics to actually teach the other ACGME competencies too!
For example, discussing ethical dilemmas can teach professionalism.

15/ In summary, remember teaching doesn't require much prep.
Look at the list in the morning and decide WHAT to teach & WHERE/HOW to teach it.
Choose teaching points that:
1⃣ you already know
2⃣ align with CURRENT patient care needs
And mix it up using the ACGME competencies!
Look at the list in the morning and decide WHAT to teach & WHERE/HOW to teach it.
Choose teaching points that:
1⃣ you already know
2⃣ align with CURRENT patient care needs
And mix it up using the ACGME competencies!

16/ To teach effectively, it’s important to establish GOALS, even for quick clinical pearls.
Next week @GStetsonMD will describe how to develop clear, focused learning objectives.
Follow @GStetsonMD & @YihanYangMD so you don't miss anything from @MedEdTwagTeam!
Next week @GStetsonMD will describe how to develop clear, focused learning objectives.
Follow @GStetsonMD & @YihanYangMD so you don't miss anything from @MedEdTwagTeam!

@threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh