This #novice anaesthesia thread is about spinal anaesthesia.
Thanks to @anaecritmed for the suggested topic.
Once again I’ve made a summary infographic. I’ll break it down as we go and direct you to some useful resources and websites for further reading
Comments welcome
1/n
Thanks to @anaecritmed for the suggested topic.
Once again I’ve made a summary infographic. I’ll break it down as we go and direct you to some useful resources and websites for further reading
Comments welcome
1/n

first off -a Comprehensive summary from THE online resource for regional anaesthesia (@NYSORA)
nysora.com/techniques/neu…
I also strongly encourage you to look at this 3-d model to visualise the spine. It helps troubleshoot failed spinal
sketchfab.com/3d-models/lumb…
2/n
nysora.com/techniques/neu…
I also strongly encourage you to look at this 3-d model to visualise the spine. It helps troubleshoot failed spinal
sketchfab.com/3d-models/lumb…
2/n
Spinals are a form of neuraxial block.
Specifically a block in the subarachnoid space.
The first reported case was by August Bier in 1898 using cocaine (Ester) who gave himself and assitant post-dural picture headache. Opiates were first added in 1901 by Racoviceanu-Pitesti
3/n
Specifically a block in the subarachnoid space.
The first reported case was by August Bier in 1898 using cocaine (Ester) who gave himself and assitant post-dural picture headache. Opiates were first added in 1901 by Racoviceanu-Pitesti
3/n

The spinal cord extends down to the conus medullaris at L1 in adults (L3 in infants)
CSF resides between the pia and arachnoid mater (subarachnoid space)
Although the arachnoid is delicate it presents a formidable barrier to drug translocation
4/n
CSF resides between the pia and arachnoid mater (subarachnoid space)
Although the arachnoid is delicate it presents a formidable barrier to drug translocation
4/n
In accessing the subarachnoid space using a midline approach we have to traverse
Skin and subcutaneous tissue
Supraspinous ligament
Interspinous ligament
Ligamentum flavum
Dura mater
Arachnoid mater
ykhoa.org/d/image.htm?im…
5/n
Skin and subcutaneous tissue
Supraspinous ligament
Interspinous ligament
Ligamentum flavum
Dura mater
Arachnoid mater
ykhoa.org/d/image.htm?im…
5/n

Sites of action of the injected drugs are:
1 - Spinal cord
2 - Spinal nerve roots
3 - Dorsal root ganglia
(c-spine for illustrative purposes)
By user:debivort - Own work, CC BY-SA 3.0, commons.wikimedia.org/w/index.php?cu…
6/n
1 - Spinal cord
2 - Spinal nerve roots
3 - Dorsal root ganglia
(c-spine for illustrative purposes)
By user:debivort - Own work, CC BY-SA 3.0, commons.wikimedia.org/w/index.php?cu…
6/n

Size, surface area and degree of myelination of nerves affect the speed and penetrance of anaesthesia
So not all nerves are blocked at identical concentrations
So not all sensory modalities are blocked at the same level
This is the premise of a differential sensory block
7/n
So not all nerves are blocked at identical concentrations
So not all sensory modalities are blocked at the same level
This is the premise of a differential sensory block
7/n

This means checking cold modality only with your ethyl chloride spray will not tell you the height at which pain is blocked. So if you use this, make sure you have gone 2 dermatomes above the level required!
8/n
8/n
How to get the right level?
The main factors determining the block height are:
Dose (volume x concentration) = MLAC
Baricity
CSF volume
Advanced Age
Extremes of Height+weight
Pregnancy
Positioning of patient
doi.org/10.1093/bjacea…
MLAC discussed here
doi.org/10.1093/bja/ae…
9/n
The main factors determining the block height are:
Dose (volume x concentration) = MLAC
Baricity
CSF volume
Advanced Age
Extremes of Height+weight
Pregnancy
Positioning of patient
doi.org/10.1093/bjacea…
MLAC discussed here
doi.org/10.1093/bja/ae…
9/n

We can tilt the patient to affect the spread under gravity of hyperbaric solutions. However after 25mins the level is fixed
10/n
10/n
The duration of the block is clearly important and affected mostly by the dose (vol x conc), the local anaesthetic, additives used.
But also by the height of block needed
Charts that compare local anaesthetic duration often include time to T10 and T4 (from NYSORA)
11/n
But also by the height of block needed
Charts that compare local anaesthetic duration often include time to T10 and T4 (from NYSORA)
11/n

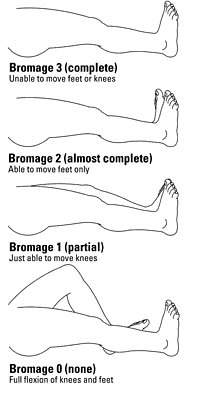
In assessing the spinal block, test three modalities:
Sensation - ethyl chloride (cold 2 levels above pain level required)
Motor - SLR (reflects lumbosacral fibres)
Sympathetic - warm touch/BP or HR changes (T1-L2 for peripheral vasodilatation, T1-T4 for cardiac fibres)
12/n
Sensation - ethyl chloride (cold 2 levels above pain level required)
Motor - SLR (reflects lumbosacral fibres)
Sympathetic - warm touch/BP or HR changes (T1-L2 for peripheral vasodilatation, T1-T4 for cardiac fibres)
12/n
Not everyone can/should have a spinal
Absolute contraindications - refusal, cardiovascular instability, active skin infection at injection site, raised ICP
Everything else is "relative"
@AAGBI has a resource for anti coagulated patients:
onlinelibrary.wiley.com/doi/full/10.11…
13/n


Absolute contraindications - refusal, cardiovascular instability, active skin infection at injection site, raised ICP
Everything else is "relative"
@AAGBI has a resource for anti coagulated patients:
onlinelibrary.wiley.com/doi/full/10.11…
13/n



Part of informed consent is explaining the risks
Quotable risks to patients come from NAP3
doi.org/10.1093/bja/ae…
nationalauditprojects.org.uk/NAP3_home
14/n
Quotable risks to patients come from NAP3
doi.org/10.1093/bja/ae…
nationalauditprojects.org.uk/NAP3_home
14/n

High spinal is a particular complication to be aware of.
It occurs as the level of the block rises and follows predictable symptoms as it affects different levels
The @AAGBI has an excellent QRH resource for managing complications. excerpt here
anaesthetists.org/Portals/0/PDFs…
15/n
It occurs as the level of the block rises and follows predictable symptoms as it affects different levels
The @AAGBI has an excellent QRH resource for managing complications. excerpt here
anaesthetists.org/Portals/0/PDFs…
15/n

Lastly a point on performing the procedure - positioning is key!
Failing to prepare = preparing to fail
Take your time in getting this right and in identifying the midline
The needle used can either be cutting or pencilpoint. Types explained here: dx.doi.org/10.1586/174344…
16/n
Failing to prepare = preparing to fail
Take your time in getting this right and in identifying the midline
The needle used can either be cutting or pencilpoint. Types explained here: dx.doi.org/10.1586/174344…
16/n

• • •
Missing some Tweet in this thread? You can try to
force a refresh







