Waveform capnography! I've been meaning to cover this for years. Finally posted an IBCC chapter on it. The chapter is pretty long (filled with subversion, physiology, and zentensivism), so here is a thread with some key points.🧵
emcrit.org/ibcc/co2/
emcrit.org/ibcc/co2/
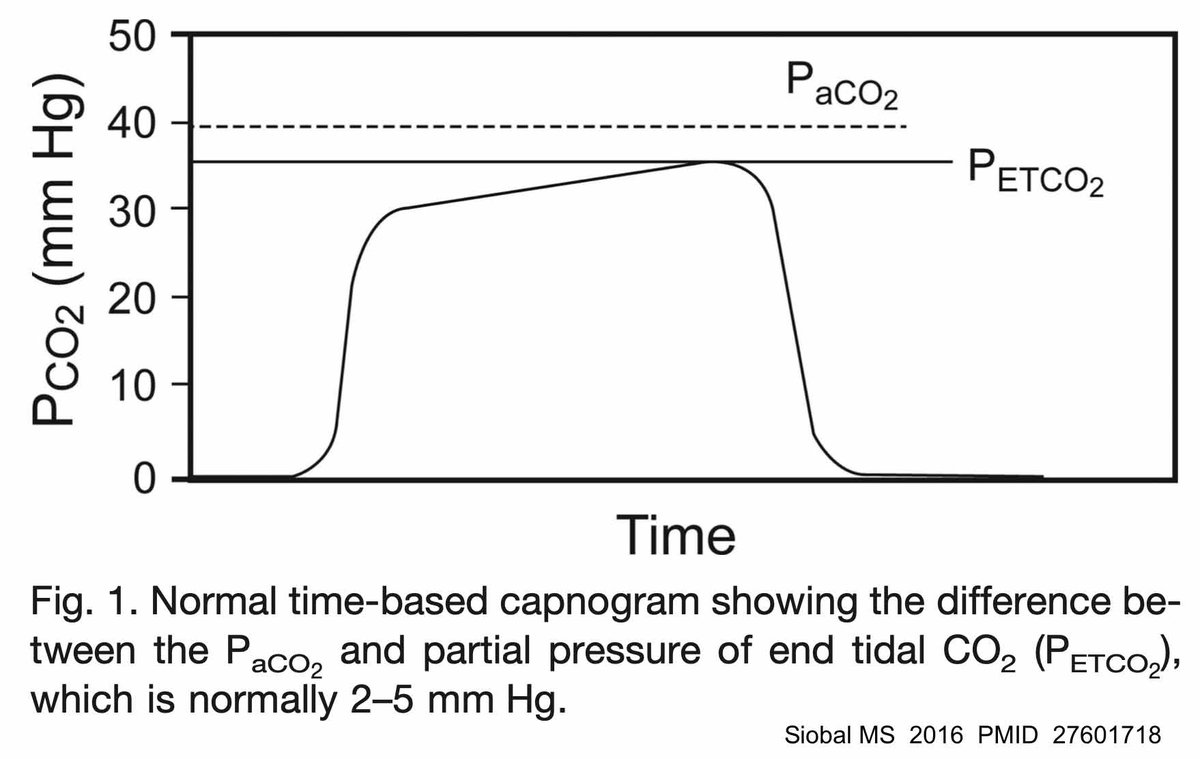
end tidal CO2 (etCO2) will ~always be lower than the arterial CO2 (b/c dead space dilutes CO2 as the patient exhales). the gap between the etCO2 and the arterial CO2 varies depending on lung function. in normal lungs, the CO2 gap is usually ~2-5 with an upper limit of ~10-15 


Imagine that we intubate a healthy patient for airway protection 2/2 intoxication. A safe pH for this patient might be ~7.2-7.5 (no good data!). To achieve this, we need an arterial pCO2 to be ~32-64 mm. So all we need to do is target an etCO2 of ~30-35 and we should be good. 

So if we don't need tight control of pH/pCO2, we could avoid ever checking a blood gas. This is a divisive concept. Anesthesiologists tend to be on board with it (b/c they often intubate w/o an ABG), whereas some pulmonologists feel that it is anathema not to check an ABG.
The neat thing about etCO2 is that if we are *wrong* (and the patient's lungs are sicker than we thought), we end up erring on the side of getting a higher pCO2 than we were targeting. and respiratory acidosis is generally well tolerated, so we tend to err towards safety.
etCO2-only ventilation monitoring does need to be reserved for a *specific* subset of patients:
👌no lung dz
👌etCO2 waveform normal & reproducible
👌patient can tolerate mild hypercapnia
👌no metabolic pH abn'l (i.e., bicarb ~normal)
👌minute ventilation requirements are normal
👌no lung dz
👌etCO2 waveform normal & reproducible
👌patient can tolerate mild hypercapnia
👌no metabolic pH abn'l (i.e., bicarb ~normal)
👌minute ventilation requirements are normal

Let's get back to the old school pulmonologists who insist on getting an ABG on every intubated patient. I did this for years and it makes no little sense. You tweak the vent aggressively for a few hours to get the perfect ABG, then *stop* monitoring ventilation at all for days🙄
etCO2 monitoring is more powerful, allowing for continuous monitoring. Key is trending the etCO2 & minute ventilation:
▪️⬆️ etCO2 & ⬇️ minute ventilation = hypoventilation
▪️⬇️ etCO2 & ⬆️ minute ventilation = hyperventilation
▪️other patterns suggest change in pt's physiology
▪️⬆️ etCO2 & ⬇️ minute ventilation = hypoventilation
▪️⬇️ etCO2 & ⬆️ minute ventilation = hyperventilation
▪️other patterns suggest change in pt's physiology

In patients who don't meet criteria for etCO2-only monitoring of ventilation (e.g. due to lung dz), the etCO2 may be correlated with ABG/VBG. *Trending* etCO2 may subsequently help monitor ventilation (while avoiding lots of blood gas measurements).
using etCO2 to reduce/eliminate blood gas measurements is #zentensivist:
🧘paying *more* attention than we used to (with careful monitoring of etCO2 & minute ventilation).
🧘eliminating unnecessary tests.
🧘greater tolerance for uncertainty.
🧘paying *more* attention than we used to (with careful monitoring of etCO2 & minute ventilation).
🧘eliminating unnecessary tests.
🧘greater tolerance for uncertainty.
There's a lot more about etCO2 in the IBCC chapter
🌬️etCO2 in cardiac arrest
🌬️etCO2 & fluid responsiveness
🌬️etCO2 & spontaneous breathing trial
🌬️basic waveform interpretation
emcrit.org/ibcc/co2/
🌬️etCO2 in cardiac arrest
🌬️etCO2 & fluid responsiveness
🌬️etCO2 & spontaneous breathing trial
🌬️basic waveform interpretation
emcrit.org/ibcc/co2/
• • •
Missing some Tweet in this thread? You can try to
force a refresh






























