1/
Once upon a time I wrote a #tweetorial about #TCDs. It ended with this great hook feat Beyonce… and… then I got distracted with other things because (⬇️)
(Thinking I don’t remember this post at all, but great! I want to read about TCDs, here you go:
Once upon a time I wrote a #tweetorial about #TCDs. It ended with this great hook feat Beyonce… and… then I got distracted with other things because (⬇️)
(Thinking I don’t remember this post at all, but great! I want to read about TCDs, here you go:
https://twitter.com/caseyalbin/status/1415386203432661001)
2/
Also, side note, can we talk about Meredith gray’s hair from that tweetorial? If you are in really in medicine and have this perfect blow-out hair, please DM me so I can know your secret.
Ok, back to #TCDs.
Also, side note, can we talk about Meredith gray’s hair from that tweetorial? If you are in really in medicine and have this perfect blow-out hair, please DM me so I can know your secret.
Ok, back to #TCDs.
3/
Takeaways from the last #tweetorial
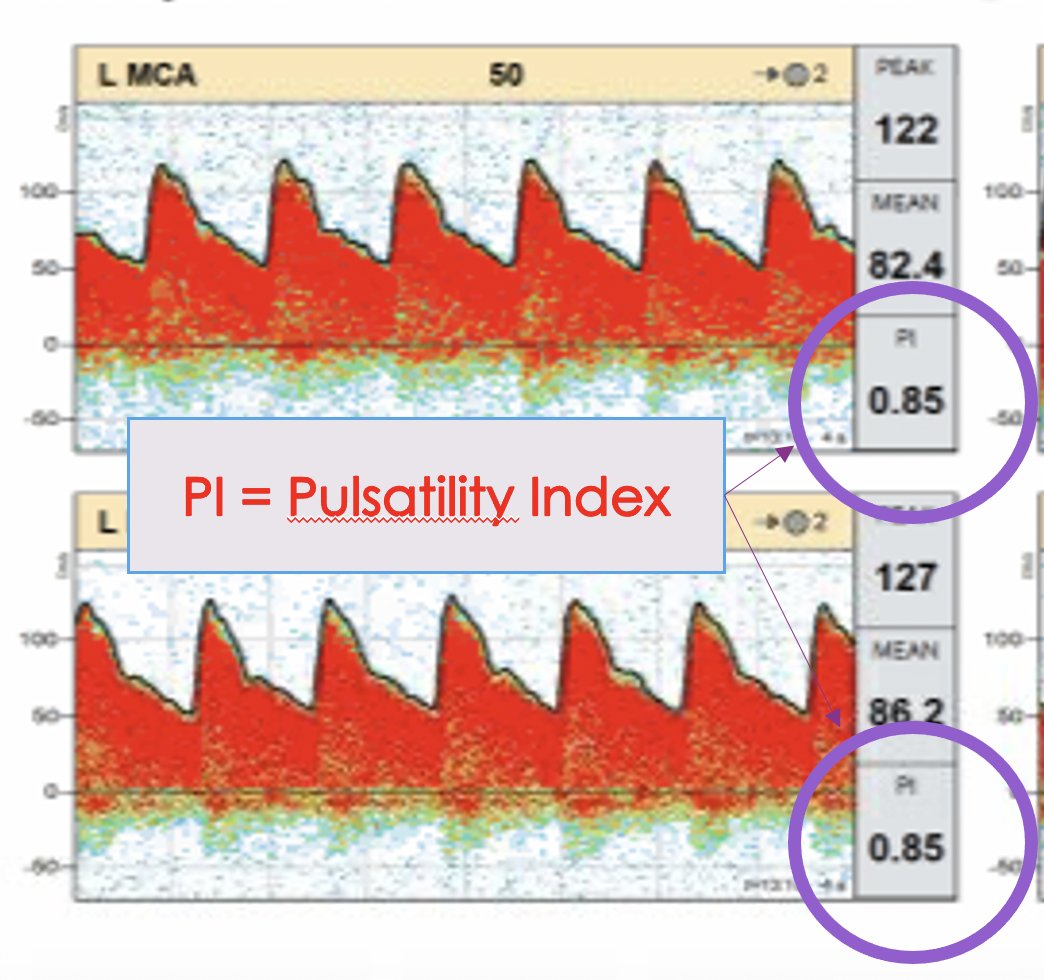
⭐️TCDs use u/s waves to calculate the velocity of intracranial blood flow
⭐️We measure systolic velocity (PSV), end diastolic velocity (EDV), Pulsatility Index (PI) & mean flow velocity (MFV)
⭐️TCDs are freq used for vasospasm monitoring
Takeaways from the last #tweetorial
⭐️TCDs use u/s waves to calculate the velocity of intracranial blood flow
⭐️We measure systolic velocity (PSV), end diastolic velocity (EDV), Pulsatility Index (PI) & mean flow velocity (MFV)
⭐️TCDs are freq used for vasospasm monitoring
4/
But as @namorrismd pointed out, while TCDs are sensitive for vasospasm (90%) and have a good NPV (92%), the PPV is low (57%).
Thus, they are a good screening test, but may not tell the whole story.
thejns.org/view/journals/…
But as @namorrismd pointed out, while TCDs are sensitive for vasospasm (90%) and have a good NPV (92%), the PPV is low (57%).
Thus, they are a good screening test, but may not tell the whole story.
thejns.org/view/journals/…

6/
What might be a more useful way to understand cerebral hemodynamics is checking for vascular reactivity w/ a CO2 challenge during TCDs (@namorris). Loss of CVR id'ed pts @ high risk for DCI (sensitivity 91%) this has also been done with acetazolamide. ja.ma/3zZ2P9o
What might be a more useful way to understand cerebral hemodynamics is checking for vascular reactivity w/ a CO2 challenge during TCDs (@namorris). Loss of CVR id'ed pts @ high risk for DCI (sensitivity 91%) this has also been done with acetazolamide. ja.ma/3zZ2P9o

6/
Why these two agents? Because both decrease the pH. Remember low pH is a potent vasodilator.
(The opposition is true of high pH… pls don’t hyperventilate the pt in vasospasm!)
Normal response to CO2 is to increase CBF.
The MCA velocities increase by 2-4% per 1 mmHg of CO2
Why these two agents? Because both decrease the pH. Remember low pH is a potent vasodilator.
(The opposition is true of high pH… pls don’t hyperventilate the pt in vasospasm!)
Normal response to CO2 is to increase CBF.
The MCA velocities increase by 2-4% per 1 mmHg of CO2
7/
Wait.
Earlier I said that we are monitoring for increased velocities to detect vasospasm…And now, I'm saying that increased velocities mean more CBF, not less??
So...Are increased velocities good or bad?
So glad you asked!
Wait.
Earlier I said that we are monitoring for increased velocities to detect vasospasm…And now, I'm saying that increased velocities mean more CBF, not less??
So...Are increased velocities good or bad?
So glad you asked!
8/
This gets back to the Lindegaard ratio. Which you’ll recall is the MCA Vmean / ICA Vmean.
🙀Vasospasm causes vasoconstriction solely in the intracranial arteries (LR increases), potentially indicating worsening CBF and a risk for DCI*
*Remember VSP is not the same as DCI
This gets back to the Lindegaard ratio. Which you’ll recall is the MCA Vmean / ICA Vmean.
🙀Vasospasm causes vasoconstriction solely in the intracranial arteries (LR increases), potentially indicating worsening CBF and a risk for DCI*
*Remember VSP is not the same as DCI
😸Lowering the pH systemically vasodilates the ICA and the MCA, allowing more blood at faster speeds through the entire system.
LR stays normal to slightly elevated
LR stays normal to slightly elevated
9/
MFV ⬆️(>~120) & LR ⬇️ (<~3-4): suspect hyperemia (usually not a bat thing, but might be problematic in situations w/ impaired cerebral auto-reg or post carotid stenting/CEA)
MFV ⬆️ (>~120) & LR ⬆️ (>~-4-6): suspect vasospasm.
(this is a gradient & clinical context matters!)
MFV ⬆️(>~120) & LR ⬇️ (<~3-4): suspect hyperemia (usually not a bat thing, but might be problematic in situations w/ impaired cerebral auto-reg or post carotid stenting/CEA)
MFV ⬆️ (>~120) & LR ⬆️ (>~-4-6): suspect vasospasm.
(this is a gradient & clinical context matters!)
10/
But what if the MFV is low?
When I started fellowship and saw a low Vmean, I'd think, "Great! this patient is not in vasospasm! everything is fine!"
But what if the MFV is low?
When I started fellowship and saw a low Vmean, I'd think, "Great! this patient is not in vasospasm! everything is fine!"
11/
That is, unfortunately, not always true.
Why?
Because there is more to TCDs than the Vmean. The waveform matters and one of the ways that that is numerically captured is the pulsatility index.
Pulsatility Index=
(Peak Systolic Vel – End Diastolic Vel)/Mean Flow Vel.
That is, unfortunately, not always true.
Why?
Because there is more to TCDs than the Vmean. The waveform matters and one of the ways that that is numerically captured is the pulsatility index.
Pulsatility Index=
(Peak Systolic Vel – End Diastolic Vel)/Mean Flow Vel.
12/
As distal resistance increases the peak systolic velocity increases.
BUT! Because the resistance is high, forward flow drastically slows during diastole.
And you get a waveform that ends up looking like this:
As distal resistance increases the peak systolic velocity increases.
BUT! Because the resistance is high, forward flow drastically slows during diastole.
And you get a waveform that ends up looking like this:

13/
Normal PI is around 1.
Something >~1.5 (or a sudden increase from prior) should clue you in to one of two things:
⭐️Distal vasospasm
⭐️Elevated ICP (causing compressive resistance on distal arteries)
Check out @ghoshal_shivani's noninvasive mini talk instagram.com/tv/CTFFrl2Hy83…
Normal PI is around 1.
Something >~1.5 (or a sudden increase from prior) should clue you in to one of two things:
⭐️Distal vasospasm
⭐️Elevated ICP (causing compressive resistance on distal arteries)
Check out @ghoshal_shivani's noninvasive mini talk instagram.com/tv/CTFFrl2Hy83…
14/
Here's an example:
47 yo W w/ aSAH HH4 post bleed day 4 w/ poor exam despite EVD.
TCD with RMCA Vmeans low (in the 40s)
All good, no vasospasm, right?
Here's an example:
47 yo W w/ aSAH HH4 post bleed day 4 w/ poor exam despite EVD.
TCD with RMCA Vmeans low (in the 40s)
All good, no vasospasm, right?

15/
Of course not -- No. This is not good at all!
The waveform here is highly abnormal with a dramatically elevated PI in the R MCA territory (other territory PIs were much more modestly elevated, near 1.2-1.5)
Of course not -- No. This is not good at all!
The waveform here is highly abnormal with a dramatically elevated PI in the R MCA territory (other territory PIs were much more modestly elevated, near 1.2-1.5)
16/
STAT CTA demonstrated severe vasospasm in the DISTAL branches of the MCA.
So, elevated PIs in this case clued us into a high distal resistance from spasm.
Pt was treated with IA therapy with mild improvement in velocities and exam.
STAT CTA demonstrated severe vasospasm in the DISTAL branches of the MCA.
So, elevated PIs in this case clued us into a high distal resistance from spasm.
Pt was treated with IA therapy with mild improvement in velocities and exam.

17/
Another example:
30 yo W aSAH HH4 with large Sylvian hematoma from rupture of an M2 aneurysm (scan ⬇️) PBD 12. Poor exam.
Another example:
30 yo W aSAH HH4 with large Sylvian hematoma from rupture of an M2 aneurysm (scan ⬇️) PBD 12. Poor exam.

18/
TCDs demonstrate pretty normal V Means
But the PIs are severely elevated in every single window (almost all >2.5)!
TCDs demonstrate pretty normal V Means
But the PIs are severely elevated in every single window (almost all >2.5)!

17/
Repeat CT scan demonstrated a new EVD tract hemorrhage.
So, here the elevated PI reflected distal downstream compression 2/2 high ICP.
Although the bleed was small, in someone who’s cerebral compliance was already maxed, this was enough to nearly result in herniation.
Repeat CT scan demonstrated a new EVD tract hemorrhage.
So, here the elevated PI reflected distal downstream compression 2/2 high ICP.
Although the bleed was small, in someone who’s cerebral compliance was already maxed, this was enough to nearly result in herniation.

18/
In this case, EVD had clotted was no longer functional, so we didn't have an invasive ICP monitor. It was the the TCDs waveforms that actually dramatically directed patient care.
Several months after the decompressive crani, this pt came back to the unit to say hi!!
In this case, EVD had clotted was no longer functional, so we didn't have an invasive ICP monitor. It was the the TCDs waveforms that actually dramatically directed patient care.
Several months after the decompressive crani, this pt came back to the unit to say hi!!
19/
Major take aways:
1⃣ TCDs = sensitive & a good screening tool for vasospasm
2⃣ pH changes vascular flow
3⃣ The pulsatility index and the TCD waveforms are ways to noninvasively look for distal vasospasm & intracranial hypertension
⭐️Great review:
pubmed.ncbi.nlm.nih.gov/31786564/
Major take aways:
1⃣ TCDs = sensitive & a good screening tool for vasospasm
2⃣ pH changes vascular flow
3⃣ The pulsatility index and the TCD waveforms are ways to noninvasively look for distal vasospasm & intracranial hypertension
⭐️Great review:
pubmed.ncbi.nlm.nih.gov/31786564/
20/ A huge thank you to @AAandersonMD who has taught me so much about #TCDs and know @aartisarwal would also have a lot to share!! thoughts? @drdangayach @iceman_ex @pouyeah @EmoryNeuroCrit @JimmySuhMD @WNGtweets @CaseyMayPharmD @EricLawson90
@threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh











