Tamponade tweetorial
1/
68m with a h/o COPD and lymphoma, presented with SOB unrelieved with home albuterol. Had an O2 sat 88% with EMS which improved with CPAP. BP 87/50 and HR 160 which improved to BP 127/70 and HR 115 after 1 L of LR. Exam had increased WOB and clear lungs
1/
68m with a h/o COPD and lymphoma, presented with SOB unrelieved with home albuterol. Had an O2 sat 88% with EMS which improved with CPAP. BP 87/50 and HR 160 which improved to BP 127/70 and HR 115 after 1 L of LR. Exam had increased WOB and clear lungs
2/
CXR showed cardiomegally which prompted cardiac #POCUS. Any significant SOB patient should have a cardiac and lung #POCUS to quickly assess for emergent pathology
CXR showed cardiomegally which prompted cardiac #POCUS. Any significant SOB patient should have a cardiac and lung #POCUS to quickly assess for emergent pathology
3/
PSLA view showed a clear large pericardial effusion. Given the patient's clear lung exam (and normal lung #POCUS), this can certainly be the cause.
PSLA view showed a clear large pericardial effusion. Given the patient's clear lung exam (and normal lung #POCUS), this can certainly be the cause.
4/
Attention is now turned to the RV free wall to look for diastolic collapse. Note that as the RV expands during diastole, the free wall is "pushed in". This is a sign of tamponade.
Attention is now turned to the RV free wall to look for diastolic collapse. Note that as the RV expands during diastole, the free wall is "pushed in". This is a sign of tamponade.
5/
While the "eyeball"method is predictive, m-mode gives a little more objectivity. M-mode is placed through the RV free wall and the mitral valve. As the MV opens during diastole (3rd squiggly line) the RV collapses (1st squiggly line), indicating diastolic RV collapse.
While the "eyeball"method is predictive, m-mode gives a little more objectivity. M-mode is placed through the RV free wall and the mitral valve. As the MV opens during diastole (3rd squiggly line) the RV collapses (1st squiggly line), indicating diastolic RV collapse.

6/
Next is the apical 4 chamber. Chamber sizes are normal. Note slight indentation in the right atrium free wall as it squeezes. This is known as "RA systolic collapse" and is a sensitive size of tamponade. You also noted echoes in the effusion near the LV. More on that later.
Next is the apical 4 chamber. Chamber sizes are normal. Note slight indentation in the right atrium free wall as it squeezes. This is known as "RA systolic collapse" and is a sensitive size of tamponade. You also noted echoes in the effusion near the LV. More on that later.
7/
"Echocardiographic pulsus paradoxus" is looked at next on the A4C. Pulse wave doppler is placed through the MV with the gate just inside the LV. This used to measure the velocity of blood entering the LV with different phases of respiration.
"Echocardiographic pulsus paradoxus" is looked at next on the A4C. Pulse wave doppler is placed through the MV with the gate just inside the LV. This used to measure the velocity of blood entering the LV with different phases of respiration.
8/
The spikes represent blood coming into the LV. Over 25% change in velocity during a respiratory cycle is considered positive. While the second velocity is not recorded here, there is clearly a large difference between the smallest and largest velocity.
The spikes represent blood coming into the LV. Over 25% change in velocity during a respiratory cycle is considered positive. While the second velocity is not recorded here, there is clearly a large difference between the smallest and largest velocity.
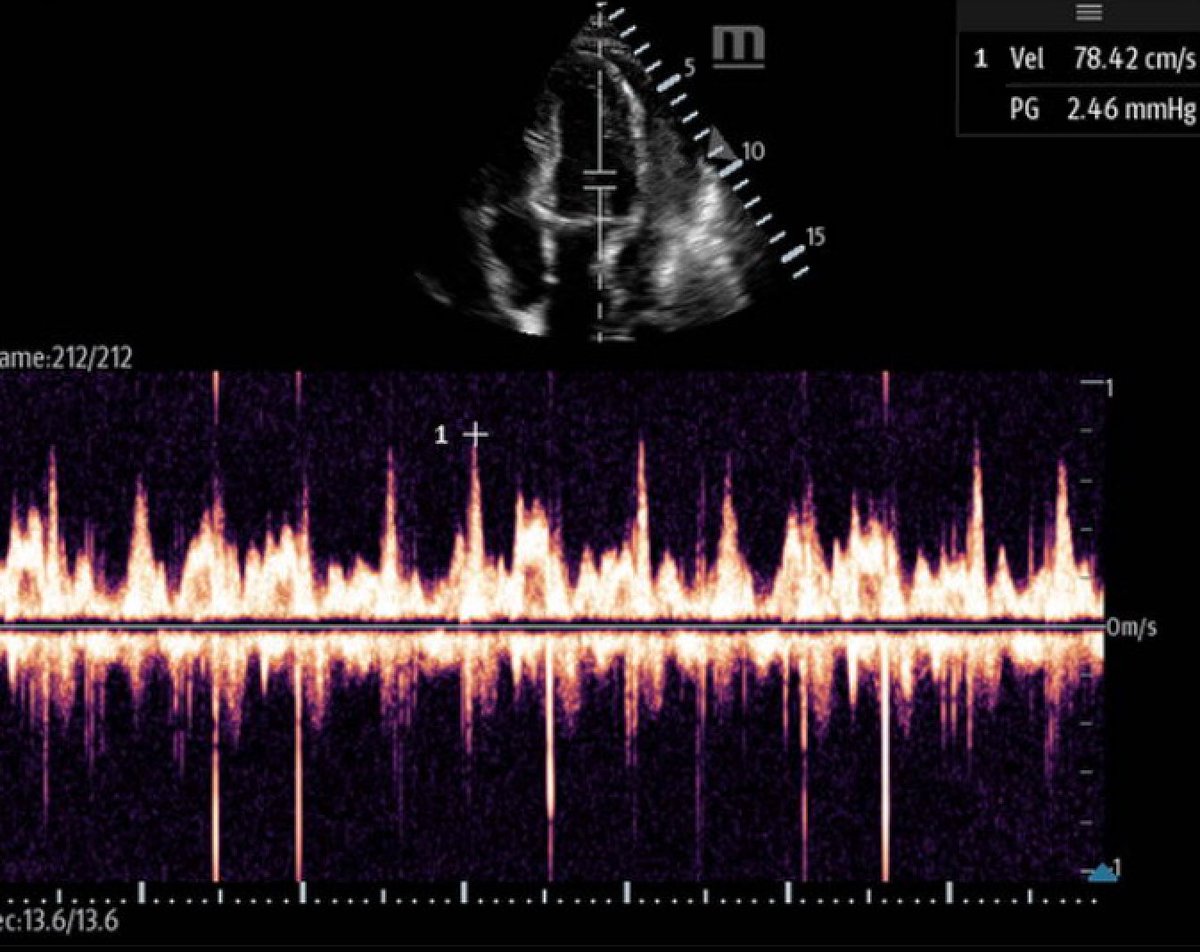
9/
The difference in this case was 50% difference. Make sure to decrease the sweep speed on the machine, which can be done while in PW mode. This slows down the recording so that you can be sure you are seeing a full respiratory cycle.
The difference in this case was 50% difference. Make sure to decrease the sweep speed on the machine, which can be done while in PW mode. This slows down the recording so that you can be sure you are seeing a full respiratory cycle.
10/
Remember those echos in the effusion? they were best seen in the PSLA around the LV. This indicates a complex effusion. Ths helps the ddc, suggesting inflammatory or infectious. Traumatic can also have echos but is not suggestive by history.
Remember those echos in the effusion? they were best seen in the PSLA around the LV. This indicates a complex effusion. Ths helps the ddc, suggesting inflammatory or infectious. Traumatic can also have echos but is not suggestive by history.
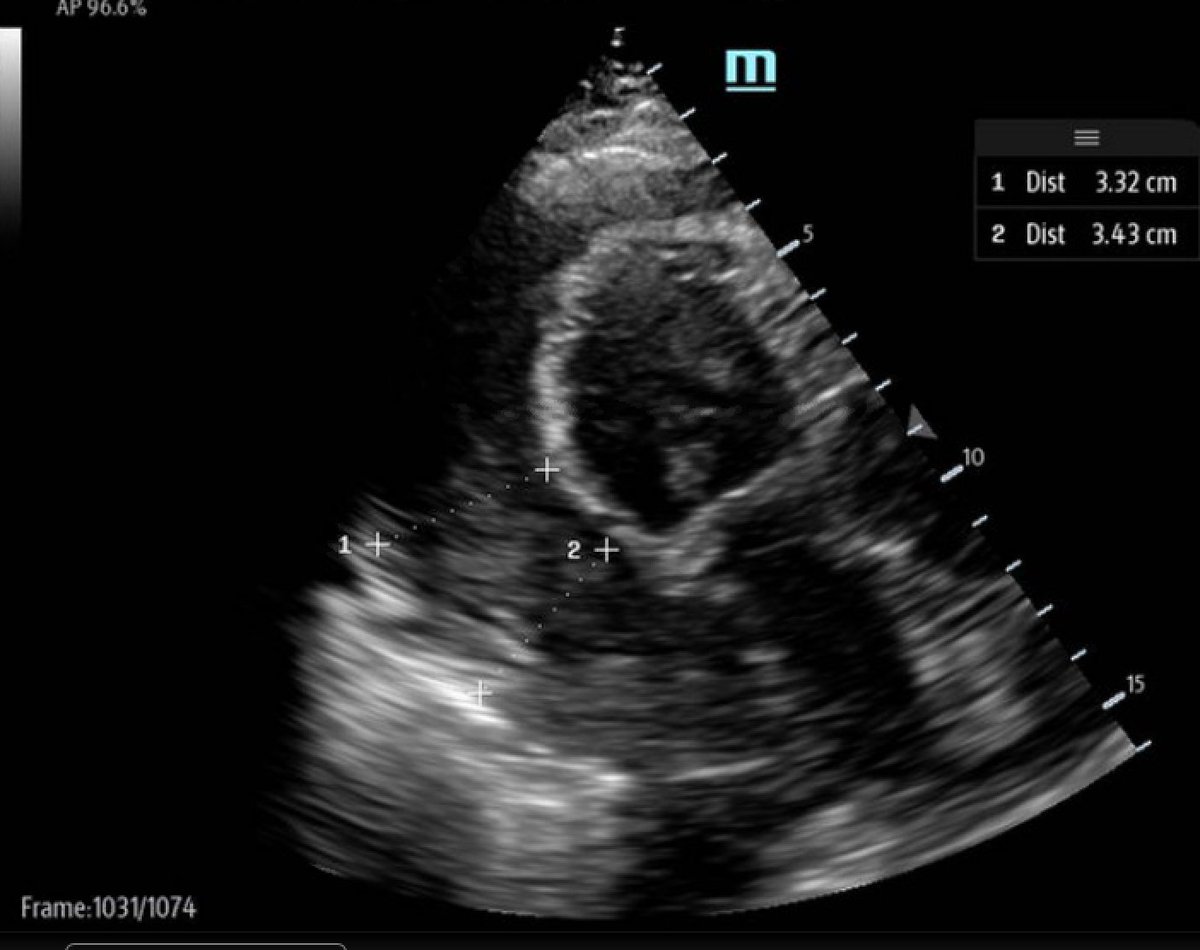
11/ A measurement of effusion size is taken at it's largest area. This is a large effusion. While rate of rise rather than absolute size is more predictive of tamponade, this assists the cardiologists so is important to measure. Measure in end diastole. 
12/
Case conclusion:
Tamponade was recognized and cardio was consulted (this was around 11 pm). Plan was for cath drainage in the AM, however (surprise surprise), the patient didn't make it that long and became more unstable during the night and taken emergently for a window.
Case conclusion:
Tamponade was recognized and cardio was consulted (this was around 11 pm). Plan was for cath drainage in the AM, however (surprise surprise), the patient didn't make it that long and became more unstable during the night and taken emergently for a window.
13/
962 cc of purulent fluid was drained.
Lesson learned:
SOB patients should get a cardiac POCUS, especially when lungs are clear. You will save a life!
962 cc of purulent fluid was drained.
Lesson learned:
SOB patients should get a cardiac POCUS, especially when lungs are clear. You will save a life!
• • •
Missing some Tweet in this thread? You can try to
force a refresh




