1/
It’s no secret what’s growing in blood.
But, the cultures won’t clear,
On valves it adheres!
Patient aphasic,
What’s with the agitation?
ESR & CRP rising!
An #Tweetorial advising:
Never overlook the spinal epidural abscess!!
#EmoryNCCTweetorials
It’s no secret what’s growing in blood.
But, the cultures won’t clear,
On valves it adheres!
Patient aphasic,
What’s with the agitation?
ESR & CRP rising!
An #Tweetorial advising:
Never overlook the spinal epidural abscess!!
#EmoryNCCTweetorials
2/
All poetry aside (pretty good tho, right?!)
Goals for the scroll (⬅️credit @sigman_md 😂):
1⃣ How difficult it can be to diagnose spiral epidural abscesses (SEA)
2⃣ What exactly is the spinal epidural space
3⃣ How these should be treated
4⃣ And why decompress?
All poetry aside (pretty good tho, right?!)
Goals for the scroll (⬅️credit @sigman_md 😂):
1⃣ How difficult it can be to diagnose spiral epidural abscesses (SEA)
2⃣ What exactly is the spinal epidural space
3⃣ How these should be treated
4⃣ And why decompress?
3/
Diagnosing SEA = super tricky. The symptoms & labs are so non-specific!
✅Back pain ⏫(but back pain--who doesn't?)
✅Fever is often present, but not always.
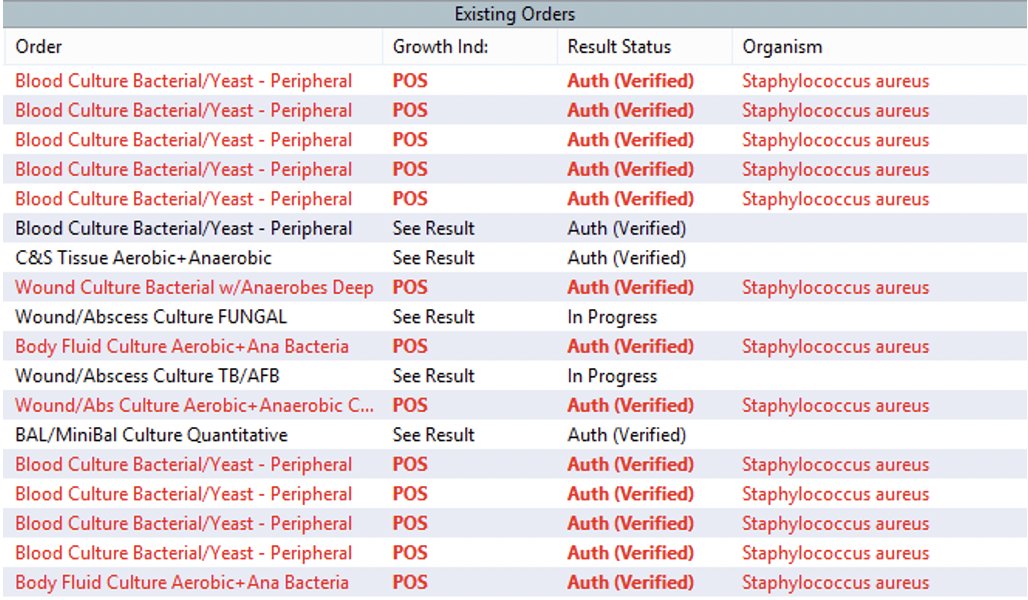
✅WBC may be elevated, but sometimes just mildly. ✅Blood cultures are only positive about 60% of the time.
Diagnosing SEA = super tricky. The symptoms & labs are so non-specific!
✅Back pain ⏫(but back pain--who doesn't?)
✅Fever is often present, but not always.
✅WBC may be elevated, but sometimes just mildly. ✅Blood cultures are only positive about 60% of the time.
4/
⭐️ESR and CRP are also nearly universally sig elevated
😑 But again...More than 1 reason for that.
So then, do I have to worry about a SEA on any patient that has backpain?
Maybe.🤷♀️
Should at least cross your mind...
⭐️ESR and CRP are also nearly universally sig elevated
😑 But again...More than 1 reason for that.
So then, do I have to worry about a SEA on any patient that has backpain?
Maybe.🤷♀️
Should at least cross your mind...
5/
Most patients have one risk factor:
👉DM, HIV, immunomodulating tx, IV drug use.🚩
👉Recent instrumentation, chronic indwelling spinal hardware, anesthetic injections, pressure sores 🚩🚩
👉And (obvi) if your patient has florid staph endocarditis and back pain… 🚩🚩🚩🚩
Most patients have one risk factor:
👉DM, HIV, immunomodulating tx, IV drug use.🚩
👉Recent instrumentation, chronic indwelling spinal hardware, anesthetic injections, pressure sores 🚩🚩
👉And (obvi) if your patient has florid staph endocarditis and back pain… 🚩🚩🚩🚩
6/
🧫Good ole sticky staph aureus is the most common culprit by far.
🧫Staph epi, other coag neg staph are problems too (prior surgery/hardware)
🧫GNRs can be found
& then of course there are some fun shout outs to mycobacteria, fungi and actinomycosis / nocardiosis in the lit.
🧫Good ole sticky staph aureus is the most common culprit by far.
🧫Staph epi, other coag neg staph are problems too (prior surgery/hardware)
🧫GNRs can be found
& then of course there are some fun shout outs to mycobacteria, fungi and actinomycosis / nocardiosis in the lit.
6/
🩸The majority are caused by hematogenous spread
🦠Direct extension of infection due to psoas abscess or vertebral osteomyelitis is the culprit for others to invade into the epidural space
Image: pubmed.ncbi.nlm.nih.gov/17093252/
🩸The majority are caused by hematogenous spread
🦠Direct extension of infection due to psoas abscess or vertebral osteomyelitis is the culprit for others to invade into the epidural space
Image: pubmed.ncbi.nlm.nih.gov/17093252/

7/
Which then may lead you to wonder… what is typically going on in the epidural space?🤔
This is the space between the vertebral ligaments (posterior longitudinal ligament/ligamentum flava) and the dura, which covers the thecal sac.
Image: nejm.org/doi/pdf/10.105…
Which then may lead you to wonder… what is typically going on in the epidural space?🤔
This is the space between the vertebral ligaments (posterior longitudinal ligament/ligamentum flava) and the dura, which covers the thecal sac.
Image: nejm.org/doi/pdf/10.105…

8/
Turns out, lots is going on here – there is fat that provides cushioning of the spinal cord and the venous plexus that drains spinal artery, as well as some smaller arteries that nourish the dura and leptomeninges.
Image: spineuniverse.com/conditions/spi…
Turns out, lots is going on here – there is fat that provides cushioning of the spinal cord and the venous plexus that drains spinal artery, as well as some smaller arteries that nourish the dura and leptomeninges.
Image: spineuniverse.com/conditions/spi…

9/
So when a lot of bacteria get in there… like seen here (ps- T1. CSF should be dark😱🔽). It’s generally… not great.
Heusner described in 1948: These infections progress through 4⃣ steps of damage
👉Pain
👉Radiculopathy
👉Weakness & Bowel/bladder dysfunction
👉 Paralysis
So when a lot of bacteria get in there… like seen here (ps- T1. CSF should be dark😱🔽). It’s generally… not great.
Heusner described in 1948: These infections progress through 4⃣ steps of damage
👉Pain
👉Radiculopathy
👉Weakness & Bowel/bladder dysfunction
👉 Paralysis

10/
So back to the staph case…
☑️Started on abx for MRSA (a must!!)
☑️Exam with no signs of myelopathy.
☑️MRI has no evidence of cord signal change.
(Just all that contrast enhancing material pus/infection surrounding the spine)
Again... 😱
So back to the staph case…
☑️Started on abx for MRSA (a must!!)
☑️Exam with no signs of myelopathy.
☑️MRI has no evidence of cord signal change.
(Just all that contrast enhancing material pus/infection surrounding the spine)
Again... 😱

11/
He’s persistently bacteremic with a high fever (not good for the stroke recovery ... another complication of the endocarditis! Gotta protect the brain!)
Stat consult to NSGY who initially were kinda like …
🤨No cord signal?
🤨No signs of myelopathy?
(nicely, of course!)
He’s persistently bacteremic with a high fever (not good for the stroke recovery ... another complication of the endocarditis! Gotta protect the brain!)
Stat consult to NSGY who initially were kinda like …
🤨No cord signal?
🤨No signs of myelopathy?
(nicely, of course!)
12/
But on re-review with an awesome chief:
More like…
“We should take him… We wouldn’t be decompressing because cord compression, but to, as you know, prevent cord ischemia from the venous congestion and potential thrombosis these epidural abscesses cause. Right?”
But on re-review with an awesome chief:
More like…
“We should take him… We wouldn’t be decompressing because cord compression, but to, as you know, prevent cord ischemia from the venous congestion and potential thrombosis these epidural abscesses cause. Right?”
13/
Also me…5 seconds later, googling “how do epidural abscesses cause damage?”
(Ps I freaking love this gif)
Also me…5 seconds later, googling “how do epidural abscesses cause damage?”
(Ps I freaking love this gif)
14/
Being totally honest:
Decompression for source control… ✔️on board
Decompression because this could progress to causing mechanical cord compression… 💯%
Decompression for of venous congestion and impending cord infarction…
Being totally honest:
Decompression for source control… ✔️on board
Decompression because this could progress to causing mechanical cord compression… 💯%
Decompression for of venous congestion and impending cord infarction…
15/
So, is that true?
Well, this was an en vogue thing to look at back in the 1930s-1970s when a lot more autopsies were being performed for spinal cord injury.
Got some airtime in NEJM (1975) (Shout out @MGHPathology, EP Richardson)
So, is that true?
Well, this was an en vogue thing to look at back in the 1930s-1970s when a lot more autopsies were being performed for spinal cord injury.
Got some airtime in NEJM (1975) (Shout out @MGHPathology, EP Richardson)

17/
So, yes. The pathophys of SEA seems to be complicated & some combination of
💪Mechanical compression
🟦Venous congestion
🟥Arterial thrombosis
👋The hand-wavy toxic effects of the organism’s endotoxins
So, yes. The pathophys of SEA seems to be complicated & some combination of
💪Mechanical compression
🟦Venous congestion
🟥Arterial thrombosis
👋The hand-wavy toxic effects of the organism’s endotoxins
18/
TL;DR summary (😂): regardless of if ur outpatient, hospitalist, ED, intensivist, neurologist:
🔥Spinal epidural abscess=critical, can’t miss dx
🔥Consciously think about it or you'll miss it
🔥Decompression has a role beyond source control & relieving mechanical compression
TL;DR summary (😂): regardless of if ur outpatient, hospitalist, ED, intensivist, neurologist:
🔥Spinal epidural abscess=critical, can’t miss dx
🔥Consciously think about it or you'll miss it
🔥Decompression has a role beyond source control & relieving mechanical compression
@EricLawson90 @drdangayach @emcrit @PulmCrit @AvrahamCooperMD @nickmmark @namorrismd @AaronLBerkowitz @aartisarwal @SatyaPatelMD @The_ASSR @EmmGeezee @EmoryNeuroCrit @ghoshal_shivani @rkchoi @CarlosdelRio7 @JenniferSpicer4 @CriticalCareNow @critconcepts @COREIMpodcast
@EM_RESUS @laxswamy @emily_fri @VizcarraJA @CajalButterfly @grepmeded @YihanYangMD @zach_london @MedTweetorials @avkwong @LITFLblog @IM_Crit_ @EM_NCC @em
• • •
Missing some Tweet in this thread? You can try to
force a refresh












