B.1.1.529 (nu) is bad news. It has an unusually high number of mutations.
And my (and Haseltine's) stated concern about molnupiravir accelerating evolution of SARSCoV2 is being discussed now.
The former makes me even more concerned about the latter.
And my (and Haseltine's) stated concern about molnupiravir accelerating evolution of SARSCoV2 is being discussed now.
The former makes me even more concerned about the latter.
https://twitter.com/michaelzlin/status/1462573071156535297
Merck claims there isn't a higher rate of viral mutations in molnupiravir clinical trial participants. But (1) this logically contradicts its stated mechanism of action and (2) we need to see the data to know the confidence level of this statement
edition.cnn.com/2021/11/23/hea…
edition.cnn.com/2021/11/23/hea…

Specifically, how could molnupiravir (Lagevrio) work by causing mutations in SARSCoV2, but when Merck sequences virus from patients taking molnupiravir they see no higher rate of mutations. Is the drug working or not?
sciencedirect.com/science/articl…
sciencedirect.com/science/articl…
Merck may simply not have looked hard enough, or there could be a higher rate of mutations but it is not a stat sig effect due to small sample sizes, so the difference is real but not detected, i.e. a Type 2 statistical error.
FDA cannot approve monupiravir (and MHRA should rescind their conditional approval) until we know for sure that the drug is not increasing mutagenesis of SARSCoV2 in patients taking it. But again that just seems logically impossible. Merck absolutely cannot have it both ways.
I couldn't find any MHRA assessment materials but FDA's AMDAC will have a public hearing on molnupiravir on 11/30. Watch this page for meeting materials to be posted, but it's possible the materials won't mention the question of mutagenized escape.
fda.gov/advisory-commi…
fda.gov/advisory-commi…
And now molnupiravir efficacy is down to 30% in the final analysis (just shows how noisy these measurements are when so few events are analyzed, h/t @logan_citizen).
Reward/risk ratio just went way down.
Hopefully the AMDAC briefing docs will be updated
Reward/risk ratio just went way down.
Hopefully the AMDAC briefing docs will be updated
https://twitter.com/EricTopol/status/1464233509820583938
Current AMDAC briefing docs use the now-incorrect 50% prevention of hospitalization, not the updated 30%.
I hope this isn't going to be another case where company lets FDA and advisors discuss early better data and forgets to point out later worse data
fda.gov/media/154421/d…
I hope this isn't going to be another case where company lets FDA and advisors discuss early better data and forgets to point out later worse data
fda.gov/media/154421/d…
The AMDAC briefing documents are now available. The FDA assessment confirms the presumed MOA being mutagenesis of the viral genome, but doesn't even mentino the possibility of escaped viruses being mutated faster (which may be the majority of cases).
fda.gov/media/154418/d…
fda.gov/media/154418/d…

This seems to be yet another example of FDA narrowly focusing on its pre-epidemic job. FDA looks for safety and efficacy for that patient at that time, not for people in general in the future. Faster viral evolution? Not their concern!
Draft questions are equally oblivious. No mention of viral mutation as a concern. I hope some better-informed advisor or staffer will raise the question.
fda.gov/media/154414/d…
fda.gov/media/154414/d…

The FDA has added an addendum reporting protection from hospitalization has dropped to 30%.
Actually the 95% CI for benefit is 1-50%. The wide CI means the 30% number is not very reliable, although it's the best possible estimate at this time.
fda.gov/media/154419/d…
Actually the 95% CI for benefit is 1-50%. The wide CI means the 30% number is not very reliable, although it's the best possible estimate at this time.
fda.gov/media/154419/d…

Even more concerning is the document reiterates mutagenicity to the patient as a topic, but again neglects to mention the possibility of mutagenicity to escaped viruses.
fda.gov/media/154419/d…
fda.gov/media/154419/d…

If this gets approved, my first question when I have to meet with strangers isn't going to be "are you vaccinated?"
Instead it's going to be, "you're haven't taken molnupiravir recently, have you?"
Instead it's going to be, "you're haven't taken molnupiravir recently, have you?"
And molnupiravir is different from remdesivir. Remdesivir worked by blocking replication entirely, not by inducing mutations. See this article entitled "Molnupiravir: coding for catastrophe". Given the authors' enthusiasm, the irony appears unintentional.
nature.com/articles/s4159…
nature.com/articles/s4159…

Dr. William Haseltine made the same points earlier than me. See below.
I'll just add we now *know* molnupiravir doesn't always kill off SARSCoV2 in people. Heck we know it only prevents hospitalization 30% of the time!
Viral mutation is a real concern.
forbes.com/sites/williamh…
I'll just add we now *know* molnupiravir doesn't always kill off SARSCoV2 in people. Heck we know it only prevents hospitalization 30% of the time!
Viral mutation is a real concern.
forbes.com/sites/williamh…

Past arguments aimed at addressing the concern over sublethal mutagenesis were in actuality less than reassuring. As in frightening. Next few posts describe quotes from advisory.com/daily-briefing…
Merck's Hazuda said "we don't see any infectious virus" in people who took the 5-day course.
We now know that that cannot possibly be true. The virus only prevents hospitalization by 30% (95% CI 1%-50%). That means most people who would get hospitalized still get hospitalized.
We now know that that cannot possibly be true. The virus only prevents hospitalization by 30% (95% CI 1%-50%). That means most people who would get hospitalized still get hospitalized.

What Hazuda said might have been true for an initial set of healthy volunteers but is clearly NOT TRUE for those people who take the drug and become hospitalized anyway. So this statement is NOT accurate and thereby NOT reassuring anymore.
Next, a virologist found 162 mutations after 30 rounds of replication in sublethal molnupiravir. That's about 5 mutations per round. When we do directed evolution of proteins, we aim for 4-5 mutations per gene per round. It's routine to find mutants with improved fitness this way 

We will often find 1 or 2 mutations out of 4-5 are beneficial and the others neutral. 5 mutations per round is not enough to guarantee loss of function of the entire virus (30,000 nt genome). The observation that "most of the mutations slowed the virus' growth" is NOT reassuring.
We need 100% of the mutant viruses to be worse. Even 0.1% of mutant viruses being better is not good enough. That 0.1% will go on to infect the next cell and propagate into unlimited numbers of viruses with higher fitness in the future.
Thus we've seen *no* proof that molnupiravir only mutates SARSCoV2 to less fit forms. Given the disaster that mutation to more virulent or evasiave forms would be, the burden must be on Merck to prove that doesn't happen.
And finally, we don't need molnupiravir anyway. It works far worse (~30% vs hospitalization) than drugs that don't cause viral mutagenesis, such as monoclonal antibodies (>70%) or protease inhibitors (89%).
In conclusion, it would be highly irresponsible to approve molnupiravir unless the possibility of sublethal accelerated viral mutagenesis is thoroughly addressed and satisfactorily rejected, especially within the target population of patients at risk of hospitalization.
BTW, no, I'm not getting paid to bash on Merck. I didn't get paid to point out J&J vaccine efficacy was low either. And neither am I anti-drug or anti-vaccine. My lab develops drugs and my kids got vaxxed within a week of their earliest possible dates.
I'd just like my children (and yours) to grow up in a world where we use vaccines and medicines effectively, and where they don't have to worry about the possibility of hypermutated viruses generated from the irresponsible use of mutagenizing drugs.
Have been busy the last few days, but figured I'd add to this thread, as the AMDAC meeting is going on right now, and FDA had uploaded new materials for that meeting that *finally* discuss the viral mutagenesis issue.
First we'll rewind a little to what was previously said in public about molnupiravir accelerating VOC evolution. Below, Haseltine explained his concerns while vague generalizations/guesses were presented for the other side (hardly assuring)
science.org/content/articl…
science.org/content/articl…

"I don’t share the alarm in this. If you force an organism to mutate more, it’s more likely to be bad for the virus" is not reassuring at all, for many reasons. One, even if "more likely" is true, it's not good enough. We need 0% chance of viruses surviving molnupiravir.
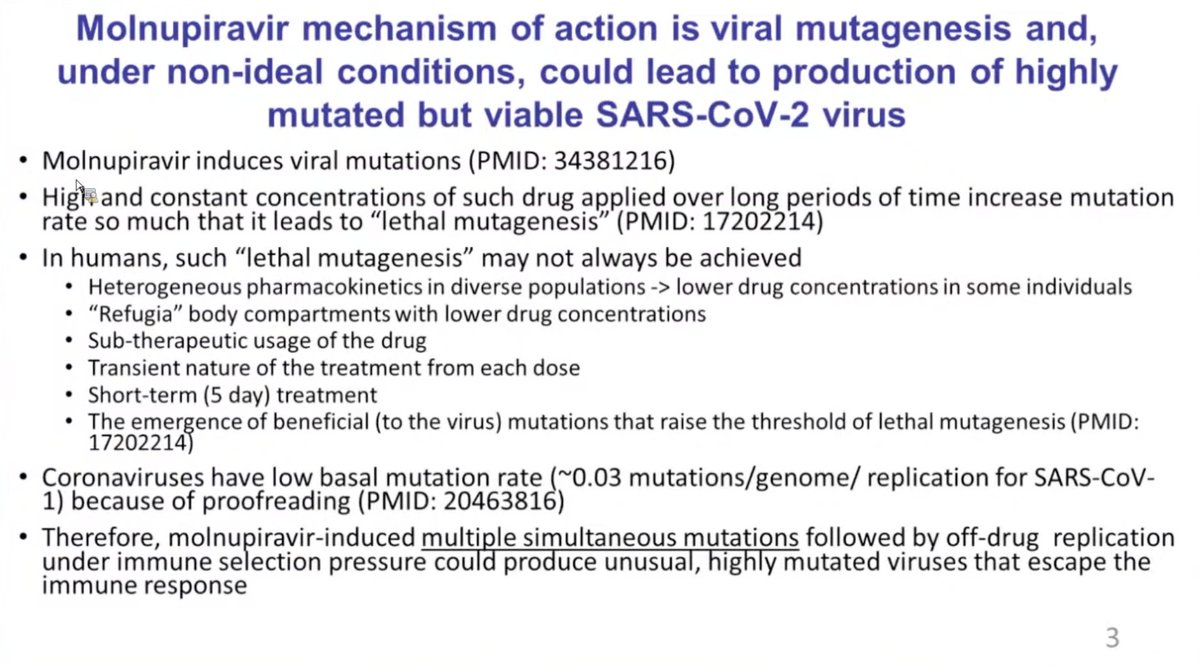
Second, it's *more* likely molnupiravir will end up creating a virus with mutations that help it evade immunity or spread, so the guess is wrong, In fact this is a mathematical certainty. As stated above, we already know that at some concentrations of the drug...
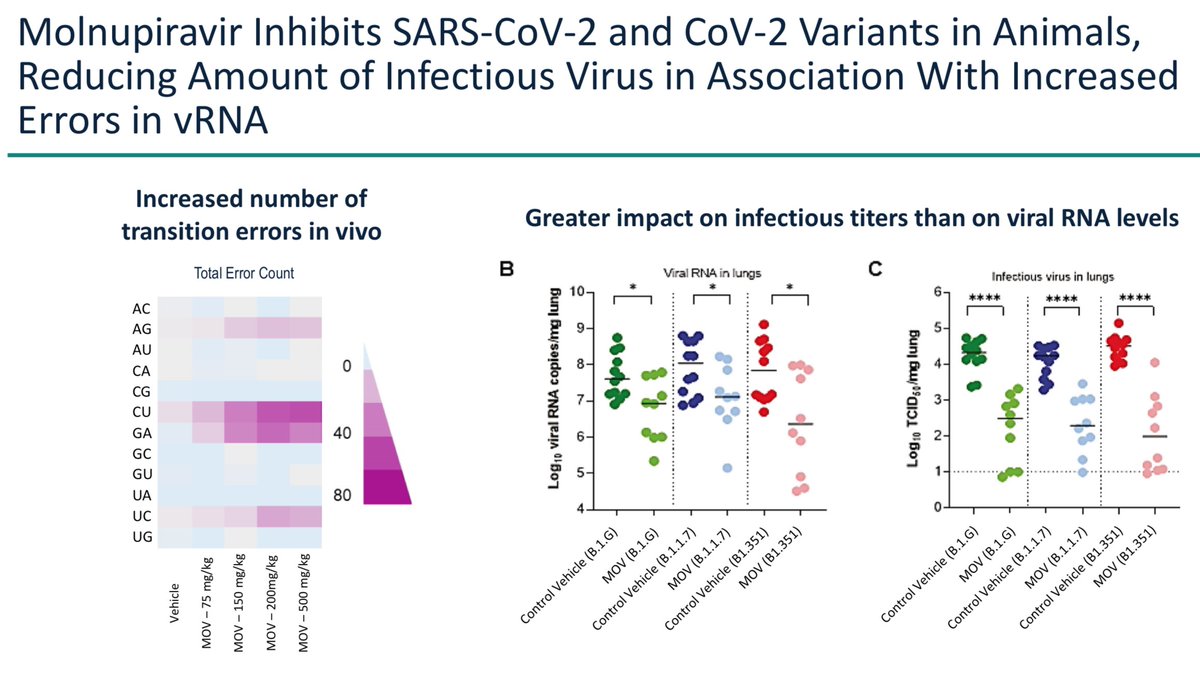
coronaviruses will pick up 162 mutations in 30 cycles, compared to their usual rate of 23 after 250 passages without drug, while reaching titers AS HIGH AS untreated virus (Fig 6 below)! If you do the math, that's about a 50-fold increase in rate. journals.asm.org/doi/10.1128/JV…
So we already have empirical evidence the drug can create mutated virus without killing it. Eventually some of those non-lethal mutations will create an advantage. This is easy enough to imagine in the case of mutations that break antibody binding sites in the spike protein,
as we are seeing now in omicron. Once there is an advantage of course that virus copy will outgrow others in the body, escape immunity, and transmit. It's the same as natural evolution, just sped up by the increased mutagenesis rate.
It's a mathematical/physical/chemical certainty that concentrations of molnupiravir that are not lethal to coronaviruses but can mutate them exist at some time or some place in treated patients. First drugs have partial efficacy at certain concentrations, it's never all or none.
At lower concentrations you see partial effects, again here expected from lower concentrations causing a few mutations. Here's the actual inhibition curve for molnupiravir (prev called NHC) on coronaviruses MHC and MERSCoV 

When you dose a drug, obviously it starts from 0 concentration everywhere in the body to some higher concentration, but it passes gradually through all concentrations in between. For oral drugs, usually it takes an hour or two to reach peak. And then it gradually falls.
If someone forgets a dose or stops taking the drug, then doses fall down below the targeted concentration. So at ramp-up and ramp-down viruses are passing through mutagenizing concentrations of molnupiravir that are also known not to kill it.
There's also the issue that not all tissues achieve the same concentration of drug. We don't take out nasal biopsies to figure out if a drug is reaching target doses in the nose; we just look at blood levels. We completely expect drug concentrations could be lower in some tissues
Finally, given the poor clinical results, the targeted dose isn't even at a level that kills virus reliably in high-risk people. So for all the reasons above, we can expect there will be viable mutated virus in patients taking molnupiravir at least some times if not most times.
When Katzourakis said, “If you force an organism to mutate more, it’s more likely to be bad for the virus", he's likely thinking in broad evolutionary terms. Coronaviruses' proofreading replicases may keep their 30,000-letter genome from mutating away to dysfunction over time.
But molnupiravir's not going to be taken by every person on earth continuously. It's just given for 5 days, and we know it only makes a 30% difference in hospitalization! So a lot of the time (maybe most) virus replicates fine with it. And once the 5 days end, or even earlier,
mutated viruses can jump to people *not* taking molnupiravir, so those viruses are now carrying a set of nonlethal mutations and ongoing mutagenesis stops.
With due respect, Katzourakis is not a biochemist, has never cultured a virus, has never studied drug concentrations in the body over time after a dose. It's inappropriate to generalize from broad principles of viral evolution to guess that "more likely" things will be fine...
if you perform short pulses of nonlethal mutagenesis on SARSCoV2 in people with immune systems, within a population of people not taking the drug, the exact environment for accelerating evolution of immunoevasion.
I'd also point out that Merck's claims on viral mutations in patients have changed over time. In the article at science.org/content/articl…, they said in people taking the drug for 5 days: "we don’t see any infectious virus". 

But later in CNN at cnn.com/2021/11/23/hea…, they said viruses did pick up mutations, but these were similar to known ones.
If Merck didn't look hard enough the first time, are they looking hard enough now?
If Merck didn't look hard enough the first time, are they looking hard enough now?

And now to today: FDA did post new documents for AMDAC. It's a mixed bag. The discussion questions still don't talk about viral mutagenesis (concentrating on the patient taking molnupiravir, not those who might get infected by newly mutated virus) 

There is one slide in the FDA briefing document raising the issue, but it's half-hearted and lacks the detailed mechanistic explanation I laid out above. 

And finally the Merck presentation. They present real data, and then proceed to draw all the wrong interpretations. It's very worrisome.
First, they show the inhibition curves. So as before with other coronaviruses, molnupiravir doesn't kill all SARSCoV2 through a wide concentration range. But it shows some activity, so clearly plenty of mutagenesis is going on at those concentrations. 

The wrong conclusion is in the green box: "high barrier to the development of resistance": They mean you can always dose >1uM and kill the virus. That's not the point at all. The point is how to prevent viruses from escaping before enough mutations accumulate to kill them.
They then show molnupiravir suppresses viral levels in animals by 100x. They're hoping the gullible think this is great. It's not remotely acceptable when you have mutations accumulating. You need zero surviving virus, whereas 1% of billions of viruses is still millions too many 
Finally they show mutations occur randomly, so obviously you are going to get new variants with altered protein functions. Yet they say because all mutations in spike were previously seen before they're not worried. This is irresponsibility of the highest order. 

They even tried to unpin molnupiravir from spike mutagenesis by saying "most mutations" were not consistent with the MOA of inducing transitions (e.g. G to A or C to U). Well it was 7 non-transitions to 5. Again, "most" isn't very reassuring. 

Anyway there's no magical reason that the virus will confine mutations to only what we've seen already. Indeed Omicron shows that there are many more possible evasive mutations than we've seen so far.
Thus Merck is denying basic mechanism and generalizing irresponsibly from partial empirical findings to incorrectly claim that viral mutagenesis is not concerning. Obviously they want to get this drug approved. But scientists and regulators must stop this dangerous effort.
BTW, should we trust that Merck has done a thorough job now? Their answers to whether mutated viruses are surviving have been:
1. No, we see no live virus
2. OK we see live virus, but the mutations are not new
3. Well, we see live virus with new mutations, but not in spike
1. No, we see no live virus
2. OK we see live virus, but the mutations are not new
3. Well, we see live virus with new mutations, but not in spike
I'm hopeful FDA will do the right thing and not approve #molnupiravir
https://twitter.com/matthewherper/status/1465800520057163782
Thank you, Dr. Hildreth.
https://twitter.com/JamesEKHildreth/status/1465806607909064705
In the AMDAC meeting, Rustem Ismagilov covered the risk of mutagenesis with slides in the public hearing session. He raised all the same concerns as me (brief mutagenesis, suboptimal drug levels in some tissues, rare events become important if advantageious) 
We came to the exact same concerns independently from basic mechanisms (Rustem is a Caltech chemistry professor). It suggests our logic is not loose but deterministic.
You can listen to his interesting/scary presentation below at 5:12:40.
You can listen to his interesting/scary presentation below at 5:12:40.
And Carl Bergstrom now comes to the same conclusions regarding molnupiravir. Low benefit, risk of creating new omicrons = absolutely not worth it. Frightening that we even consider letting big pharma play with fire.
https://twitter.com/CT_Bergstrom/status/1467611446053851145?t=TqZ4e5ynFSpny7jnIGAXtg&s=19
And an excellent thread dissecting the contradictory and data-free nature of Merck's claims that escape of enhanced viruses would be unlikely.
In the end, there is no evidence of unlikely, and even if true, unlikely is not good enough
In the end, there is no evidence of unlikely, and even if true, unlikely is not good enough
https://twitter.com/chasewnelson/status/1466331830345293827?t=rBvQ_b52lGAPqXQtJFbBgg&s=19
There are many incisive observations in that thread, including this frightening one showing Merck isn't even committed to the lethal part of lethal mutagenesis
https://twitter.com/chasewnelson/status/1466398342494048264
France shows leadership and rationality. They have rejected molnupiravir, citing correctly the 30% reduced hospitalization vs 80% for mAbs, and lack of proof mutated virus has been eliminated. Image from Google translate
h/t @Valio_ch
has-sante.fr/jcms/p_3304161…
h/t @Valio_ch
has-sante.fr/jcms/p_3304161…

Hoping this can stop the go fever. We need antiviral drugs but we don't need molnupiravir.
In fact with only 30% fewer hospitalizations (~3% absolute benefit in the treatment group) while mutating viruses in the ~7% who still get worse, it could be more proviral than antiviral
In fact with only 30% fewer hospitalizations (~3% absolute benefit in the treatment group) while mutating viruses in the ~7% who still get worse, it could be more proviral than antiviral
Spoke with a virologist physician friend yesterday (well known person) who says the feeling in the community is molnupiravir is pretty bad and shouldn't be approved. Yet you wouldn't know that from reading the news, which recently seemed to only quote virologists supporting it.
So there is healthy disagreement here, and I have reasons to believe it is occurring in the FDA as well, but the press has not captured it. I chalk this up to a "go fever" in anticipation of dramatic events such as the first oral antiviral drug developed during for COVID19
That is, reporters look for the next big thing and act as emotional communicators rather than analyzers. They mean to capture the mood by getting enthusiastic quotes, which are easily available from the people involved in the drug (their participation makes them part of the news)
The go fever gets so ingrained that interestingly even clear signs of disagreement (e.g. 10 out of 23 advisors voting no, raising concerns that weren't even asked, despite public pressure to say yes) are brushed aside as irrelevant minority views.
Only clear binary events like a HAS rejection can break the narrative. But this can engender confusion and disappointment in those who believed it. Thus when reporting on scientific matters with public health consequences, it would be nice if reporters do not to add to "go fever"
Oh Denmark, how could you. Looks like our work is not done getting people to realize the consequences. Nothing against Merck, but patients shouldn't be taking a drug that's inferior to other options, and nobody can afford to make the epidemic worse.
reuters.com/world/europe/d…
reuters.com/world/europe/d…
Controversial in Denmark too. People are waking up.
If we're lucky this will end up like Aduhelm: approved but everyone's smart enough to avoid it.
medwatch.com/News/Pharma___…
If we're lucky this will end up like Aduhelm: approved but everyone's smart enough to avoid it.
medwatch.com/News/Pharma___…
• • •
Missing some Tweet in this thread? You can try to
force a refresh










