New @JAMAInternalMed w/ @DKorenstein: #ChoosingWisely has had huge reach in shaping conversations - and efforts to reduce - #lowvaluecare. We unpacked the types and expected impact of U.S. #ChoosingWisely recommendations, w/ some surprising finds. 🧵1/ jamanetwork.com/journals/jamai…
In 2012, @ABIMFoundation @ConsumerReports launched #ChoosingWisely - asking professional societies to list low-value services to avoid. CW intentionally let docs set their own priorities to leverage their professional values, but some worried about unintended consequences. 2/
In our qualitative analysis of all 626 U.S. physician recs, most recs identified low-value imaging and lab studies in patients w/ chronic conditions or w/ risk factors alone. Few tackled (for example) visits/hospitalizations or services at end-of-life (missed opportunities?) 3/ 

Most recs (64%) were revenue-neutral for the society’s member physicians. Sometimes (2%), following the rec would even earn $ for member physicians. Meanwhile, the lowest-cost services (<$200 per unit) were the largest share of named services, and this share grew over time. 4/ 

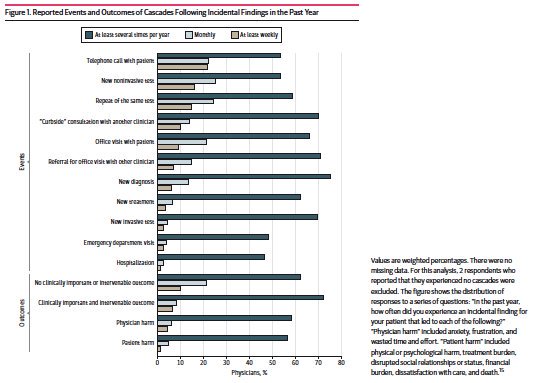
The recommendations varied widely along 4 dimensions of impact: The named low-services had varying $ and size of affected populations. Promisingly, 45% of identified low-value services had high direct harm potential and 62% had high cascade potential. 5/ 



Of course, recs only useful if acted on (per @betsyqcliff, multi-pronged interventions work best👇). Given how hard interventions are, we hope our analyses can inform new recs + help clinical leaders/policymakers/payers prioritize services to target. 6/ milbank.org/quarterly/arti…
Grateful for a thoughtful editorial by Niloofar Latifi @RFRedberg and Deb Grady. And to our non-Twitter coauthors: Meredith Rosenthal @HarvardHPM and Nitya Thakore @nyugrossman 7/
jamanetwork.com/journals/jamai…
jamanetwork.com/journals/jamai…
cc @ChoosingWiselyCA @WolfsonD @CarrieHColla @jnmafi @A_Schwa @JMichaelMcW @CostsofCare @neel_shah @oakes_ah @TomRadomskiMD @Kelsey_Chalmers @FutureDocs @BenHarder @LownInstitute 8/
• • •
Missing some Tweet in this thread? You can try to
force a refresh