I am going to try to recap my recent grand rounds on race and GFR in a few #tweetorials. Here is the third one. You can find the presentation files and a video of me presenting at pbfluids.com/2021/12/the-ne……… 1/10
In the 1980's the hot idea in nephrology was low protein diets to preserve GFR. The NIH funded a Big Science study to test the theory, the Modification of Diet in Renal Disease study, MDRD. The study was a mess and fell on its face, but they did collect a lot of cool data! 2/10
Among that data was iothalamate clearances which are a really good approximation of GFR. So Andy Levey and friends took those data and combined it with age, gender, and race to come up with the MDRD formula. 3/10 

This was the original sin, the place where nephrology started to use race to calculate eGFR. Why did they do it? You can see the from the data that Black people (open circles) tended to have higher Cr for the same GFR. 4/10
And just a year earlier a study had been published showing black people had higher serum creatinine than white people. This study had no idea what people's GFRs were. They just found higher creatinine in Black people. 5/10 

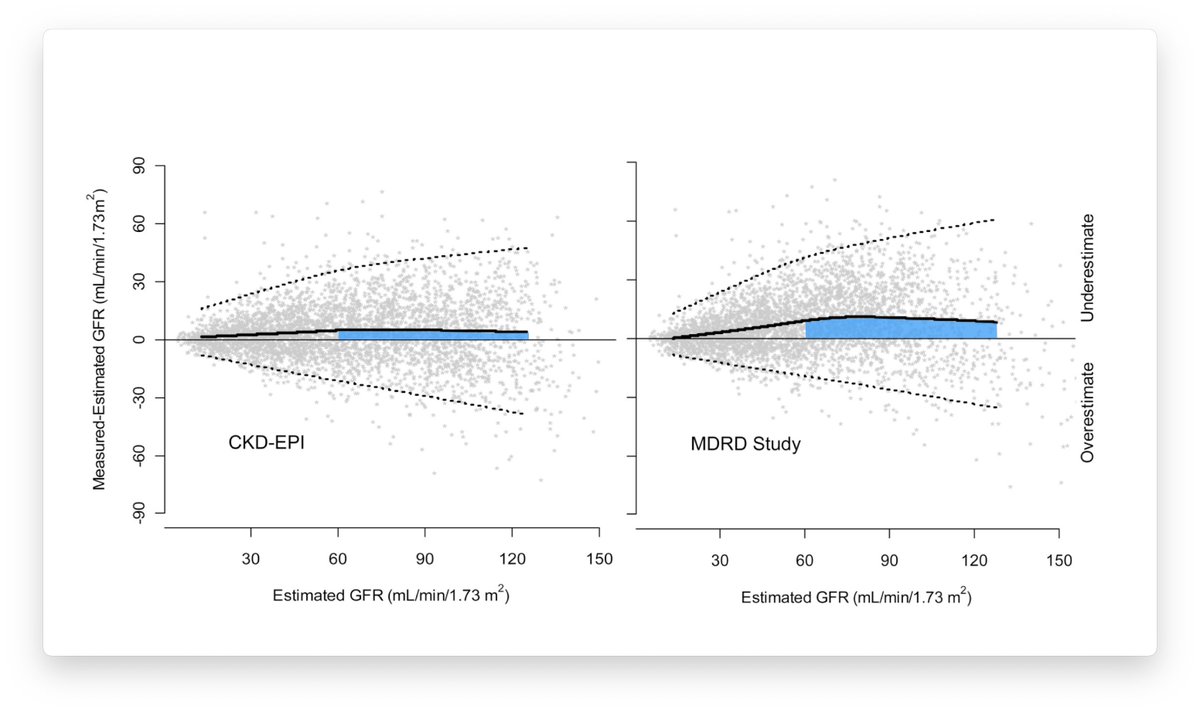
MDRD had other problems. It underestimated kidney function in people without kidney disease. This was a big problem when screening people to be kidney donors. It also had few black people and even fewer people with diabetes (and zero people on insulin) 6/10 

But the equation business was a good racket and in 2009 Level and Co came back with the CKD-EPI formula which corrected or improved many of the problems with MDRD. 7/10 

CKD-EPI is way more complex than previous formulas. It includes a technique called a knot to allow it to change the slope at low creatinines to try to improve accuracy at high GFRs. 8/10
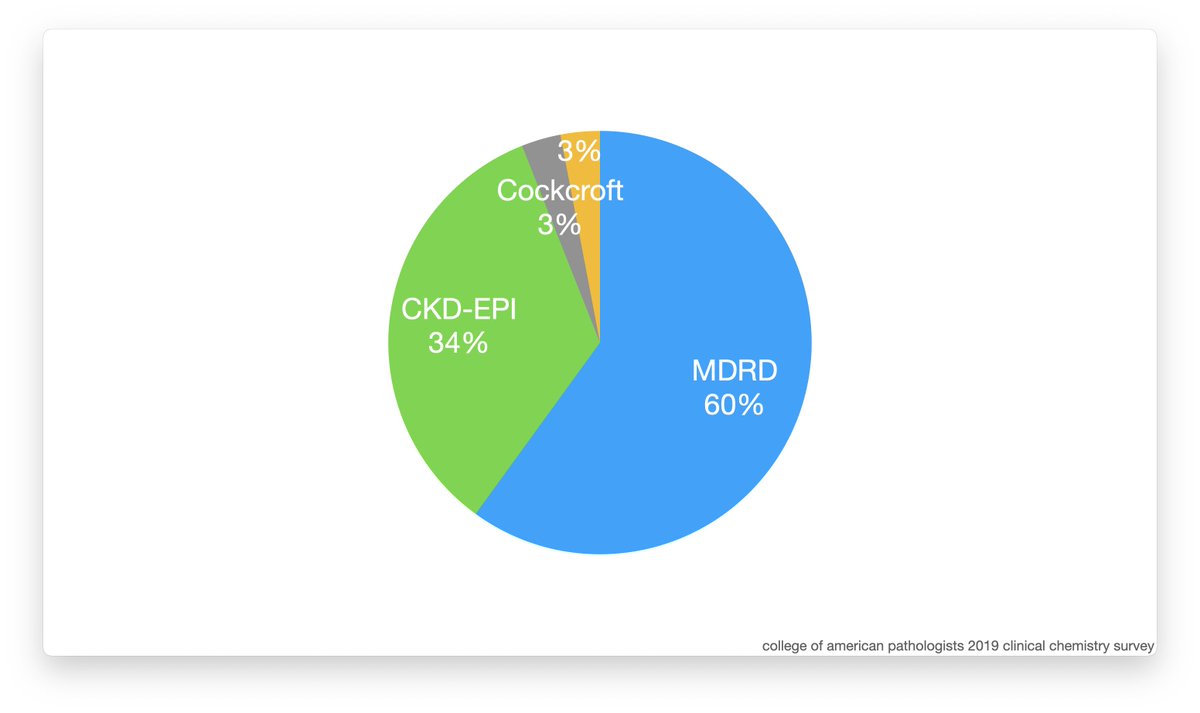
With the larger number of Black people the race adjustment shrank by about a quarter from 21% to 16%. Up until September of 2021 this was the formula people were supposed to use but a survey of clinical labs in 2019 found that 60% still used MDRD! 10/10 


• • •
Missing some Tweet in this thread? You can try to
force a refresh