1/
A pt w/ ESRD on HD, a fib on coumadin is transferred after a 2 wk hosp for SDH/contusions + ESBL PNA w/ status epilepticus
Scan ⬇️
AEDs: fPHT 100mg Q8H, LEV 1g BID, LAC 100mg BID, VPA 750mg BID + propofol 30, midaz 5.
Admission VPA level 13 (tx range 50-~100)
🤔🤔🤔
A pt w/ ESRD on HD, a fib on coumadin is transferred after a 2 wk hosp for SDH/contusions + ESBL PNA w/ status epilepticus
Scan ⬇️
AEDs: fPHT 100mg Q8H, LEV 1g BID, LAC 100mg BID, VPA 750mg BID + propofol 30, midaz 5.
Admission VPA level 13 (tx range 50-~100)
🤔🤔🤔

2/
Whats going on… That’s a 15mg/kg/day dose… why is the VPA level so low?
Whats going on… That’s a 15mg/kg/day dose… why is the VPA level so low?
3/
VPA is a great AED.
But a @medtweetorial #tweetorial, on how in the critically ill, this drug often becomes problematic and complicated.
#EmoryNCCTweetorials.
VPA is a great AED.
But a @medtweetorial #tweetorial, on how in the critically ill, this drug often becomes problematic and complicated.
#EmoryNCCTweetorials.
4/
Back to the poll choices:
1️⃣ is the VPA being chewed up by fPHT?
I’m sure @theABofPharmaC & @jimmySuhMD are going to do an incredible collab about VPA & PHT.
🛑Spoiler: they do not play nicely together.
Back to the poll choices:
1️⃣ is the VPA being chewed up by fPHT?
I’m sure @theABofPharmaC & @jimmySuhMD are going to do an incredible collab about VPA & PHT.
🛑Spoiler: they do not play nicely together.
5/
In short: VPA displaces PHT from plasma protein binding sites
This significantly ⬆️ FREE phenytoin (as it did in this case, see ⬇️).
But you might not detect this if you are just monitoring TOTAL phenytoin levels, which can stay the same or EVEN DECREASE!
In short: VPA displaces PHT from plasma protein binding sites
This significantly ⬆️ FREE phenytoin (as it did in this case, see ⬇️).
But you might not detect this if you are just monitoring TOTAL phenytoin levels, which can stay the same or EVEN DECREASE!
6/
But PHT can also ⬇️ VPA, and the effect is unpredictable.
So -- This is a plausible explanation, but the DRAMATICALLY low VPA would be a bit unexpected.
VPA+fPHT is just a headache. If you really must use, follow free levels closely.
But PHT can also ⬇️ VPA, and the effect is unpredictable.
So -- This is a plausible explanation, but the DRAMATICALLY low VPA would be a bit unexpected.
VPA+fPHT is just a headache. If you really must use, follow free levels closely.
7/
2️⃣ Is it VPA and warfarin?
No. [Obvi] this patient’s warfarin had been reversed before the burr holes…
But VPA + warfarin can cause issues:
🌟VPA can ⬆️ warfarin by ⬇️ protein binding.
🌟VPA is also an inhibitor of CYP 2C9 = ⬆️ Warfarin
2️⃣ Is it VPA and warfarin?
No. [Obvi] this patient’s warfarin had been reversed before the burr holes…
But VPA + warfarin can cause issues:
🌟VPA can ⬆️ warfarin by ⬇️ protein binding.
🌟VPA is also an inhibitor of CYP 2C9 = ⬆️ Warfarin
8/
Thanks @MeganRx1 for putting together this awesome chart for the #acuteneurologysurvivalguide. (BTW I swear is going to be published in 2022, hopefully by springtime…).
As you can see warfarin + AEDs also = headache.
Thanks @MeganRx1 for putting together this awesome chart for the #acuteneurologysurvivalguide. (BTW I swear is going to be published in 2022, hopefully by springtime…).
As you can see warfarin + AEDs also = headache.

9/
So DOACS for patients on AEDs then?
Sadly, those can be tough too. PHT, PHB, & CBZ sig induce the metabolism of DOACs and may result in therapeutic failure.
🛑 Avoid combination of PHT, PHB, or CBZ with DOAC anticoagulants 🛑
So DOACS for patients on AEDs then?
Sadly, those can be tough too. PHT, PHB, & CBZ sig induce the metabolism of DOACs and may result in therapeutic failure.
🛑 Avoid combination of PHT, PHB, or CBZ with DOAC anticoagulants 🛑
10/
3⃣Was it just VPA wasn’t being absorbed?
Well that would have been true given the state of the gut ⬇️😳But, the VPA was being given IV.
I know that its pentobarbital that gets the bad rap for GI issues, but I find that ileus is a frequent #statusproblem even w/o this med
3⃣Was it just VPA wasn’t being absorbed?
Well that would have been true given the state of the gut ⬇️😳But, the VPA was being given IV.
I know that its pentobarbital that gets the bad rap for GI issues, but I find that ileus is a frequent #statusproblem even w/o this med

11/
4⃣Carbapenem + VPA?
🛎️Bingo!
Carbapenems hate VPA, the whole VPA treatment.
Now, please don’t ask why, no one quite knows the reason.
4⃣Carbapenem + VPA?
🛎️Bingo!
Carbapenems hate VPA, the whole VPA treatment.
Now, please don’t ask why, no one quite knows the reason.
12/
Actually, the reason is probably the activation of VPA glucuronidation by carbapenems. pubmed.ncbi.nlm.nih.gov/18058328/
VPA is sig (60-90%) ⬇️ w/in 24–72 hrs of carbapenem administration!
It may take 1 – 4 *weeks* for VPA levels to recover (even if only 1 dose of abx is given!)
Actually, the reason is probably the activation of VPA glucuronidation by carbapenems. pubmed.ncbi.nlm.nih.gov/18058328/
VPA is sig (60-90%) ⬇️ w/in 24–72 hrs of carbapenem administration!
It may take 1 – 4 *weeks* for VPA levels to recover (even if only 1 dose of abx is given!)

13/
This can definitely tip a pt back into status - seen it happen😳. But, this has also (so creatively) been harnessed for good!
Got a patient with VPA toxicity or overdose?
Meropenem to the rescue.
Srsly, case report here:
pubmed.ncbi.nlm.nih.gov/31980292/
This can definitely tip a pt back into status - seen it happen😳. But, this has also (so creatively) been harnessed for good!
Got a patient with VPA toxicity or overdose?
Meropenem to the rescue.
Srsly, case report here:
pubmed.ncbi.nlm.nih.gov/31980292/

14/
Finally - The other issue that comes up with VPA is that about ~35% of patients develop hyperammonemia.
Mechanism involves a decrease in carnitine serum concentration (I’m sure @capt_ammonia could explain)!
Finally - The other issue that comes up with VPA is that about ~35% of patients develop hyperammonemia.
Mechanism involves a decrease in carnitine serum concentration (I’m sure @capt_ammonia could explain)!
15/
*Most* pts are asymptomatic, but hyperammonemia encephalopathy/cerebral edema can develop requiring IV L-carnitine 100mg/kg IV x1 f/b 15mg/kg Q4-6H (dosing from peds lits) pubmed.ncbi.nlm.nih.gov/17496767/
For asymptomatic pts can use PO l-carnitine 1000-3000mg/day in divided doses.
*Most* pts are asymptomatic, but hyperammonemia encephalopathy/cerebral edema can develop requiring IV L-carnitine 100mg/kg IV x1 f/b 15mg/kg Q4-6H (dosing from peds lits) pubmed.ncbi.nlm.nih.gov/17496767/
For asymptomatic pts can use PO l-carnitine 1000-3000mg/day in divided doses.
16/
Take aways: VPA is a great sz drug but:
💥Does not play nicely with PHT or warfarin
💥Can disappear with even a single dose of a carbapenem
💥Commonly causes hyperammonemia which is usually asymptomatic, but not always
⏸️Use with caution & monitoring in the critically ill.
Take aways: VPA is a great sz drug but:
💥Does not play nicely with PHT or warfarin
💥Can disappear with even a single dose of a carbapenem
💥Commonly causes hyperammonemia which is usually asymptomatic, but not always
⏸️Use with caution & monitoring in the critically ill.
@drdangayach @namorrismd @phil_bilodeau @sigman_md @AaronLBerkowitz @aszelikovich @EricLawson90 @rkchoi @PulmCrit @emcrit @Tracey1milligan @RebeccaFasanoMD @SubinMatthews @neudrawlogy @ghoshal_shivani @EmoryNeuroCrit @CajalButterfly @reverendofdoubt @adamdavidthomas
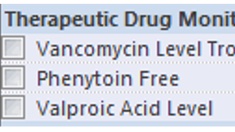
whoops twitter cropped some images!
This is the important one for tweet 5.
One day I am going to write a typo-free tweetorial with no misplaced links, no formatting/line issues, no mis-numbered tweets... that day was not today😂.
This is the important one for tweet 5.
One day I am going to write a typo-free tweetorial with no misplaced links, no formatting/line issues, no mis-numbered tweets... that day was not today😂.

• • •
Missing some Tweet in this thread? You can try to
force a refresh











