Yesterday I gave grand rounds lecture at @NJHealth about the Omicron Variant: molecular biology, epidemiology, and clinical pearls.
Here's the video & link to download my slides.
🎥
📂 onepagericu.com/blog/grand-rou…
Here's the video & link to download my slides.
🎥
📂 onepagericu.com/blog/grand-rou…
Google says AH-MUH-KRAN is 🇺🇸 & OH-MU-KRON is 🇬🇧
Oversimplified..
In ancient Greek, there were 2 letters pronounced similarly:
Ω made a long Oooo - it was called big O or O Mega
Ο made a short Oo - it was called little O or O Micron
Thus, OH-MI-KRON is probably more accurate
2/
Oversimplified..
In ancient Greek, there were 2 letters pronounced similarly:
Ω made a long Oooo - it was called big O or O Mega
Ο made a short Oo - it was called little O or O Micron
Thus, OH-MI-KRON is probably more accurate
2/

To understand Omicron, we need to understand pandemic surveillance:
A sick person 🤒 gets COVID tested.
The (+) results get sequenced (depending on where in the 🌎 ) & published to @GISAID (or other platform).
Sequences are used by researchers globally, such as @nextstrain.
3/
A sick person 🤒 gets COVID tested.
The (+) results get sequenced (depending on where in the 🌎 ) & published to @GISAID (or other platform).
Sequences are used by researchers globally, such as @nextstrain.
3/

Using @nextstrain to analyze those surveillance sequences we can watch the evolution of Omicron unfold:
Note the appearance of variants, particularly Delta in Summer 2021.
Omicron appears in October/November 2021.
On November 26, the WHO declared it a variant of concern.
4/
Note the appearance of variants, particularly Delta in Summer 2021.
Omicron appears in October/November 2021.
On November 26, the WHO declared it a variant of concern.
4/
Omicron has ~50 mutations (compared to the original strain) but >30 of them are in one gene: the Spike Protein
This is worrisome because the Spike (S) protein binds to ACE2. It's also what our immune system "sees" & makes Ab against
👀 at covariants.org for more
5/
This is worrisome because the Spike (S) protein binds to ACE2. It's also what our immune system "sees" & makes Ab against
👀 at covariants.org for more
5/
🔬 Let's look under the hood at the Spike protein mutations:
~15 in the receptor binding domain --> these *might* cause immune evasion
H655Y, N679K, P681H --> furin cleavage site mutations likely ⬆️ transmission
Q498R & N501Y --> tighter ACE2 binding, likely ⬆️ transmission
6/
~15 in the receptor binding domain --> these *might* cause immune evasion
H655Y, N679K, P681H --> furin cleavage site mutations likely ⬆️ transmission
Q498R & N501Y --> tighter ACE2 binding, likely ⬆️ transmission
6/
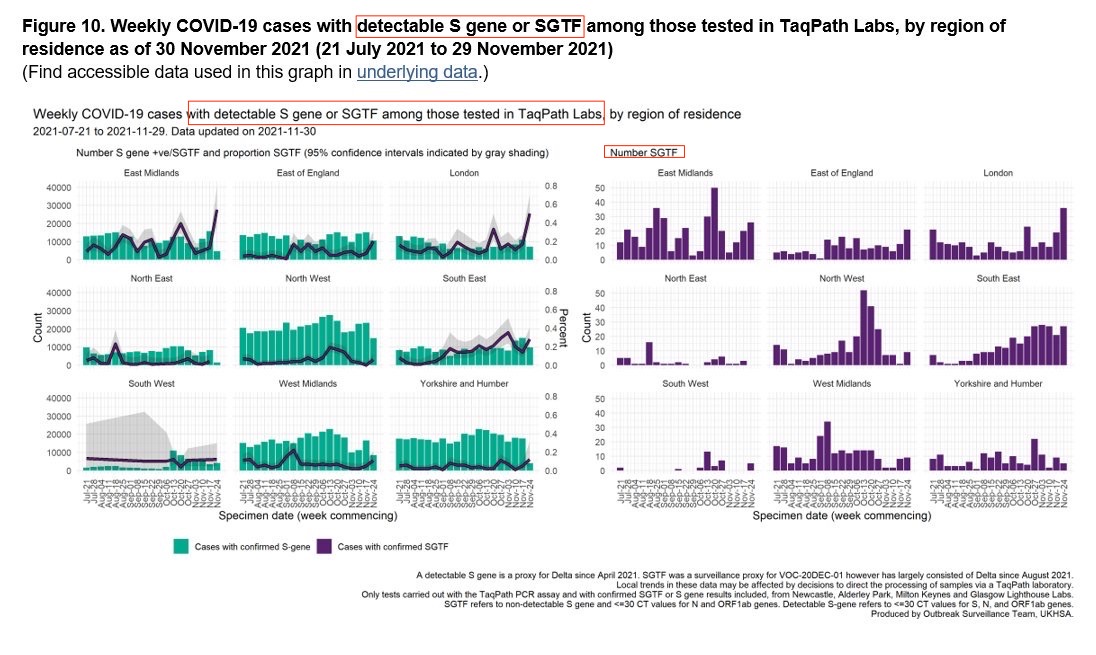
One mutation is actually useful:
The TaqPath test amplifies the S gene using PCR.
In omicron the S gene won't amplify because of deletion of 2 residues (H69-, V70-). We call the failure to amplify S Gene Target Failure (SGTF).
👉🏻You may see "SGTF" as a surrogate for Omicron
7/


The TaqPath test amplifies the S gene using PCR.
In omicron the S gene won't amplify because of deletion of 2 residues (H69-, V70-). We call the failure to amplify S Gene Target Failure (SGTF).
👉🏻You may see "SGTF" as a surrogate for Omicron
7/


Because sequences are available, the effect of the mutations can be studied in vitro & in silico
Redd et al found that despite the spike protein mutations virtually all T-cell epitopes were preserved, suggesting the virus hasn't evaded T cell immunity
biorxiv.org/content/10.110…
8/
Redd et al found that despite the spike protein mutations virtually all T-cell epitopes were preserved, suggesting the virus hasn't evaded T cell immunity
biorxiv.org/content/10.110…
8/

Another lab (Garcia-Beltran et al) found that pseudovirus particles made with the Omicron mutant spike protein were significantly more able to infect ACE2 expressing 293T cells
2x as infectious as the Delta spike and 4x the original
medrxiv.org/content/10.110…
That's worrisome..
9/
2x as infectious as the Delta spike and 4x the original
medrxiv.org/content/10.110…
That's worrisome..
9/

• • •
Missing some Tweet in this thread? You can try to
force a refresh
































