Let’s talk about natural immunity (NI) versus vaccine-induced immunity (VI) to SARS2. This has become controversial. If you survive COVID19 infection, what does that mean, immunologically and practically (given current state of knowledge and current state of the pandemic)? 1/
This is a SUPER long thread (with recent research) on a topic that has become weirdly politicized (as I learned – though I should have known with anything COVID19-related! – after my recent interview with @SamHarrisOrg ). So buckle up. 2/
I also mention this topic of natural versus vaccine-induced immunity in this 17-minute interview with @hari on @AmanpourCoPBS released last night. 3/
Bottom line: natural immunity is probably *somewhat less* effective at preventing serious COVID19 compared to vaccine immunity, or possibly *just as* effective. But this depends on many details: how sick you got, your age, the variants in circulation, and follow-up duration. 4/
Plus (and this is crucial) in order to get NI, you must survive an infection! It’s not a rational plan to say “I’ll just get immunity naturally rather than get vaccinated.” The whole point of vaccination is to give you immunity without running the (non-trivial!) risk of death. 5/
So, *given current variants*, and given the follow-up times so far available (less than a year), I would say VI is better than NI for two reasons: 1) you don’t have to run risk of death to get it, and 2) if you get VI, it’s probably slightly better than NI. 6/
This conclusion depends a lot on what any new variants do to us. For instance, while VI might be better than NI for the original strain, that might not be the case for newer strains. This means the story may change as the variant landscape changes, or with new booster shots. 7/
Now and in the future, we must go where the data take us. That is how science works. “When the facts change, I change my mind. What do you do, sir?”
Such a good quote! quoteinvestigator.com/2011/07/22/key… 8/
Such a good quote! quoteinvestigator.com/2011/07/22/key… 8/
Information on the efficacy of natural immunity is also crucial to things like allocating scarce vaccines in poor countries (why jab already immune people?) and to issues like social restrictions (if naturally immune have good protection, they should not be restricted). 9/
In #ApollosArrow (amazon.com/Apollos-Arrow-…), I note that it is possible that – unusually for a pathogen (though there is precedent, e.g., for tetanus and HPV) – the vaccines might provide superior immunity to natural infection. 10/ 

And here is a nice short November 2020 COVID commentary mentioning a range of pathogens in which, in some cases, VI is indeed better than NI (although, again, usually this is the other way around) by @EricTopol & DR Burton in @NatureMedicine nature.com/articles/s4159… 11/
Benefit of NI is old topic. In antebellum NOLA, people who were immune to yellow fever – by having survived this deadly disease which could kill 8% of population – had special status (they were “acclimated”). academic.oup.com/ahr/article-ab… Now we just get a vaccine for this scourge. 12/
Still, to be clear, and based on the review below, I think that those with (documentable) natural immunity should be treated as if they have been vaccinated and should not be discriminated against. 13/
However, from a public health policy point of view, this might not be easy to implement, and it might not actually be optimal from a collective viewpoint (it’s logistically easier to just try to vaccinate everyone, for instance). 14/
With that preamble, let’s look at current research: 1) head-to-head epidemiological studies of NI vs VI, 2) epi studies of NI, 3) epi studies of VI, 4) in-vitro studies of natural vs vaccine-induced antibodies and of cellular immunity, and 5) studies of having both NI and VI. 15/
An October 2021 @CDCgov review assessed NI vs VI studies, and concluded that VI is probably superior. cdc.gov/coronavirus/20… 16/
This @CDCgov review, based on then-available evidence & conditions, concluded that 1) mRNA vaccines lead to more consistent and higher initial antibody response, and 2) NI had efficacy against infection of 80-93% at six months, probably somewhat lower than VI (Pfizer) of 91%. 17/
For *serious disease*, this @CDCgov review concluded, VI at six months had efficacy in range of 84-96%, which is somewhat higher than that conferred by having survived natural infection (NI). 18/
In general, antibody titers rise more rapidly and reach higher levels among those with more serious COVID. In a sense, a vaccine can therefore emulate a more serious case of COVID, but without the risk. This may be one reason VI is indeed better than average NI. 19/
This also means that, if you want to rely on having been naturally infected to have good immunity, you had to have had a bad case of COVID19. Having had a mild case is unlikely to be as good as having had a vaccine. 20/
Less effective vaccines may indeed be more like natural infection (which is also in keeping with the super-immunity of the mRNA vaccines). 21/
But the story of NI versus VI is complicated, and the “literature is still young” as scientists say. 22/
Most studies conclude that protection after natural infection is durable, at least to about the longest follow-up we now have, which is about 12 months. 23/
Studies of NI can face a methodological problem. Most were done early in pandemic when testing was minimal, so asymptomatic cases were not detected. This means that the efficacy of NI was inflated since cases with weak immunity after exposure were not included in the studies. 24/
A September 2021 meta-analysis of 7 studies from US, Israel, & UK concluded that “natural immunity in COVID-recovered individuals is, at least, equivalent to the protection afforded by full vaccination of COVID-naïve populations." medrxiv.org/content/10.110… [thread continues] /25 


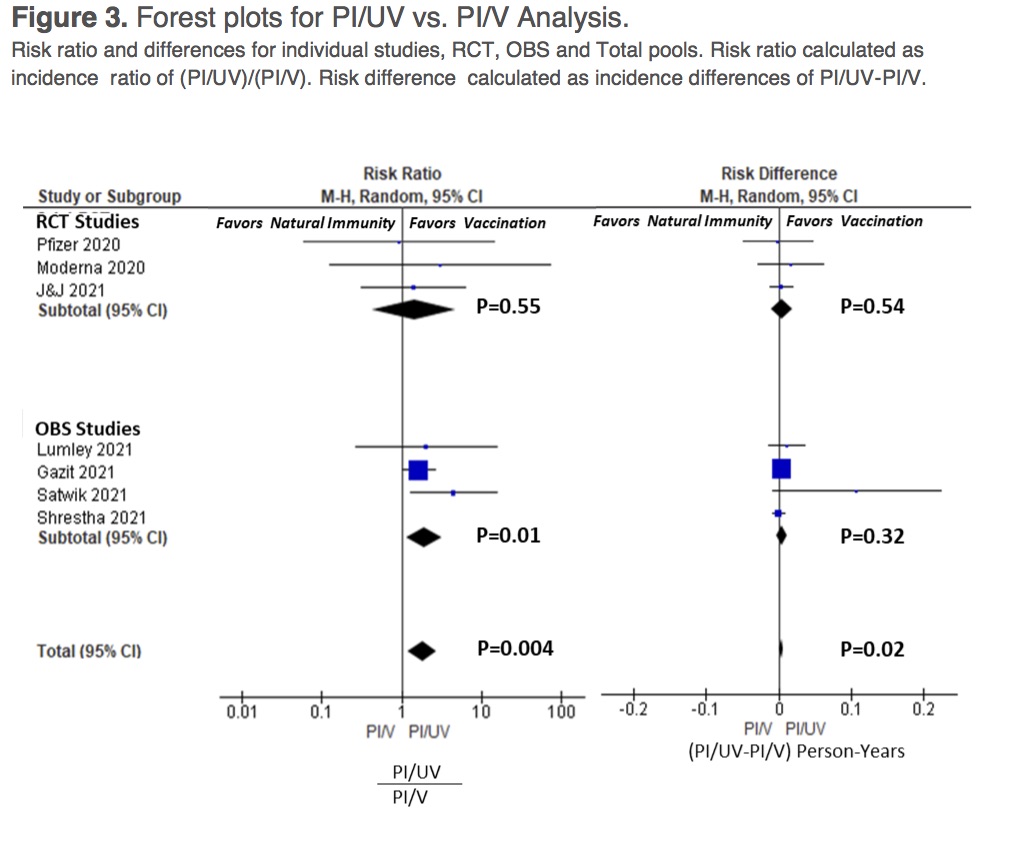
A (controversial) November 2021 analysis of 187 US hospitals found that, among 7,348 (baroquely chosen) patients hospitalized with COVID-like illness, 5.1% of those with a history of vaccination actually had COVID and 8.7% of those with prior COVID had COVID again. 26/
That is, the odds of getting COVID-19 where *higher* in previously infected patients (NI) than among fully vaccinated patients (VI). cdc.gov/mmwr/volumes/7… 27/
Said differently, the study found (in population of 7,348 hospital patients) that, of 413 cases of test-positive COVID, 324 (78%) were vaccinated & 89 (22%) had prior COVID. But in 6,935 test-negative control patients, 6,004 (87%) were vaccinated & 931 (13%) had prior COVID. 28/
In essence, this is a “case control study,” meaning that cases of COVID are compared (in terms of prior exposure to vaccination/infection) to ostensibly *otherwise similar* ppl without COVID (the controls – ppl who were sick with respiratory disease in same place & time). 29/
Choice of controls is *always* the crucial thing in such studies because it can drive the results (one can stack deck this way). Choice in this study (ppl hospitalized with COVID-like illness) seems OK. (But for a critique, see: brownstone.org/articles/a-rev… via @MartinKulldorff) 30/
An August 2021 study from Israel (medrxiv.org/content/10.110…) found that those getting the Pfizer vaccine (in January or February of 2021) had a 13-fold *increased* risk of getting infected (with delta, in the summer of 2021) compared to those with prior natural immunity. 31/
There are many strengths to this Israeli study, including the fact that it was a population-based cohort study that used an electronic database to capture both the relevant exposures and the outcomes. 32/
But there were many technical limitations too that worried me. There was evidence of imbalance in relevant covariates (e.g., the vaccinated people had more chronic diseases, despite matching on age, sex, and SES). 33/
Also, many cases were dropped due to lack of suitable matches. In key analysis, we go from 673,676 vaccinated & 62,883 naturally immune subjects to 16,215 of each. No data re these ppl is given. Comparison is made in a particular group where there is “support in the data.” 34/
Also, maybe vaccinated people took more social risks and this is why they had more infections? Or those with prior infection, having seen COVID up close, exercised more caution during follow-up? We cannot be sure. Of course, that is whole point of vaccination: to set us free. 35/
This Israeli study also found evidence that a person having *both* infection and vaccination was superior in preventing subsequent COVID infection (i.e., VI+NI > NI). 36/
An August 2021 study from India (papers.ssrn.com/sol3/papers.cf…) also found that prior infection was substantially *better* than vaccination (with AstraZeneca or an Indian inactivated-virus vaccine bharatbiotech.com/covaxin.html ) at preventing re-infection (during a period of delta). 37/
In 11,405 health care workers, protective efficacy of prior infection against symptomatic infection was 86% (95%CI 77-92%). In the absence of prior infection, vaccine efficacy (of these *non-mRNA* vaccines) against symptomatic infection during delta wave was 32% (24–39%). 38/ 

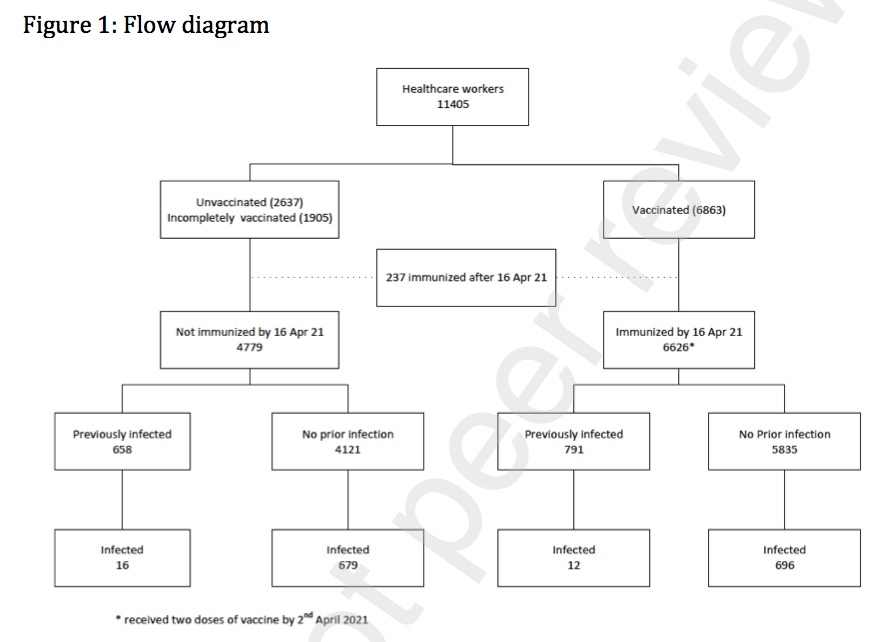

One odd finding in this study is the very low vaccine efficacy, which worked in favor of natural immunity benefit. This may relate to vaccines used, because other work finds higher efficacy (e.g., in UK, the AZ vaccine had 67% efficacy against delta (nejm.org/doi/full/10.10…). 39/
This Indian study also found evidence that having both infection and vaccination was superior. Vaccination combined with prior infection provided 91.1% (95%CI 84.1%-94.9%) efficacy in preventing subsequent COVID infection (i.e., VI+NI > NI) 40/
Another head-to-head comparison of NI versus VI in the UK, released October 2021, found that two doses of either Pfizer or AstraZeneca provided a very *similar* level of protection to previous natural infection during the Delta-dominant period. ons.gov.uk/peoplepopulati… 41/ 

Now, moving on, other studies have assessed NI and VI separately, i.e., not in the same population at the same time. We can also use these numbers to make (somewhat crude) comparisons across studies, times, and samples. 42/
A well executed study of 25,661 health care workers in UK, via @TheLancet, found that prior SARS2 infection (in the last six months of 2020, prior to vaccines) was associated with 84% (81-87%) lower risk of infection at median of 7 months follow-up. thelancet.com/article/S0140-… 43/ 

An April 2021 study in Qatar of nearly 200,000 people exposed to the virus in late 2020 found that natural immunity was 95% effective against re-infection for at least seven months. thelancet.com/journals/eclin… 44/ 

An October 2021 @JAMAInternalMed study in Italy found that during follow-up (mean 280 days, to Feb 2021), there were 5 SARS2 reinfections (0.31%) in cohort of 1,579 previously infected ppl & 528 in 13,496 uninfected ppl (~94% efficacy post adjustment) jamanetwork.com/journals/jamai… 45/ 

A February 2021 study from Austria found there were 40 tentative re-infections in 14,840 COVID-19 survivors (0.27%) and 253,581 infections in 8,885,640 ppl in general population (2.85%). The unadjusted efficacy of NI against re-infection is ~91% here. onlinelibrary.wiley.com/doi/10.1111/ec… 46/
A November 2021 study in the USA of nearly 150,000 ppl exposed to the virus in March-August 2020 concluded that protection offered by prior infection was 82% (95%CI: 77-86%) and against *symptomatic* infection was 85% (78-89%) at roughly 8 months. pubmed.ncbi.nlm.nih.gov/33718968/ 47/
A very nice March 2021 study in Denmark via @TheLancet in a population of 4M people concluded that infection during the first surge (before June 2020) was protective during the second surge later that year. thelancet.com/journals/lance… 48/
In this Danish study, protection against repeat infection was 81% (95%CI: 75-85). There was no evidence of waning over time (3-6 mos follow-up 79% vs ≥7 mos follow-up 78%). However, for those >65 years, observed protection against repeat infection was just 47% (95%CI: 25-63) 49/
Given this level of protection from prior infection (81%), the authors conclude that vaccination of previously infected individuals is sensible, “because natural protection, especially among older people, cannot be relied on.” [thread continues] 50/
Real-world studies of vaccine efficacy (VE), to supplement original RCT’s showing power of vaccines (especially mRNA vaccines, which have VE of ~95%), have also been conducted, analogous to foregoing studies of natural immunity. These generally show high levels of VE. 51/
Effectiveness of two @pfizer doses was 93.7% (95% CI, 91.6-95.3) for alpha variant and 88.0% (85.3-90.1) for delta variant. With @AstraZeneca vaccine, effectiveness of two doses was 74.5% (68.4-79.4) for alpha and 67.0% (61.3-71.8) for delta. nejm.org/doi/full/10.10… 52/ 

One multi-hospital USA study (in March-July 2021) found vaccine efficacy of mRNA vaccines against hospitalization (with both alpha and delta) to be 86% (95%CI: 82-88%) at median of two months after second dose: cdc.gov/mmwr/volumes/7… 53/
A multi-site study of frontline workers found vaccine efficacy of mRNA vaccines against infection to be 80% (95%CI: 69-88%). Efficacy during delta was 66% compared with 91% during the months preceding delta. cdc.gov/mmwr/volumes/7… 54/
A multi-site October 2021 USA study of 3.4M people in @TheLancet found that, for fully vaccinated individuals, @pfizer vaccine effectiveness against infection was 73% (95%CI: 72–74) and against COVID19-related hospital admission was 90% (89–92). thelancet.com/journals/lance… 55/
This excellent study also found that vaccine effectiveness against infection declined from 88% (95% CI 86–89) at first month after full vaccination to 47% (43–51) at 5 months, but protection against serious illness stayed very high (>80% in all ages). 56/ 

Importantly, vaccine effectiveness against hospital admissions for infections with the delta variant for all ages was high overall (93% [95% CI 84–96]) up to 6 months. thelancet.com/journals/lance… 57/ 

A @NEJM study in Qatar of mRNA vaccine efficacy (against beta and delta from January-August of 2021) found efficacy against serious illness reached 66% by 3 weeks after second dose and >96% by 8 weeks, persisting at this level for a few months. nejm.org/doi/full/10.10… 58/ 

Another @NatureMedicine study in Qatar found effectiveness against delta-induced severe, critical, or fatal disease to be 93.4% (95%CI, 85.4–97.0%) for @pfizer and 96.1% (71.6–99.5%) for @moderna_tx ≥ 14 d after second dose. nature.com/articles/s4159… 59/
In sum, NI yields efficacy of 80-95% and VI of 80-96%, across range of studies with huge variety of circumstances. These rates are very similar. But the better studies point to an advantage for vaccines. And other lab evidence, below, also suggest this. At least at present. 60/
Now, yet another way to assess possible relative efficacy of NI and VI is via in vitro studies of sera from infected and vaccinated people against old or new variants. While not as real-world as actual epidemiological studies, considered above, they are more controlled. 61/
A March 2021 @FrontImmunol review of in vitro efficacy of mRNA vaccines found they “can elicit specific antibody titers and neutralizing antibody concentrations above that observed in COVID-19 convalescent serum in first 100 days after vaccination.” frontiersin.org/articles/10.33… 62/
Another modeling study of in vitro efficacy via @NatureMedicine finds that the mRNA vaccines out-perform convalescent serum (at least up to roughly 8 months) nature.com/articles/s4159… 63/ 
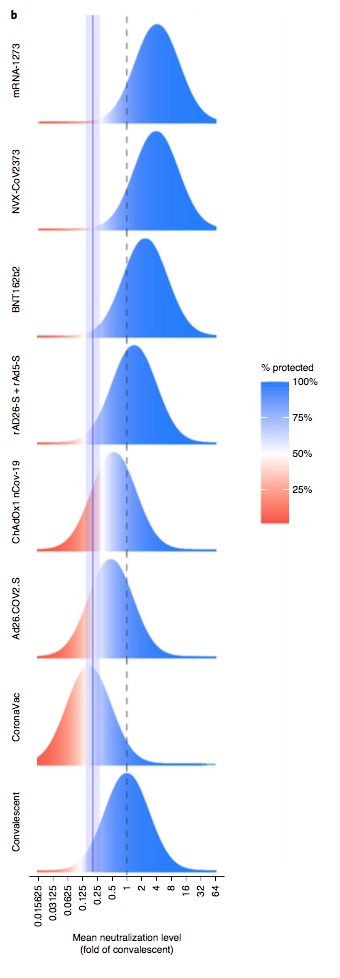
A @NEJM analysis of antibodies in response to the @moderna_tx vaccine 6 months after administration found it comparable to that seen in convalescent COVID patients through about 8 months. nejm.org/doi/10.1056/NE… 64/ 

An August 2021 analysis of 2,653 individuals fully vaccinated with mRNA vaccine and 4,361 convalescent patients found higher IgG antibody titers in vaccinated individuals than in convalescent individuals. pubmed.ncbi.nlm.nih.gov/34462761/ 65/
But in vaccinated subjects, antibodies decreased by 40% per month, while in convalescents they decreased by <5% per month. Six months after vaccine, 16.1% subjects had level below seropositivity threshold, while only 10.8% of convalescents were below threshold after 9 months. 66/
But cellular immunity in response to both natural infection & vaccination is also key, along with long-term follow-up (which is not yet possible). One @ScienceMagazine study found memory B cells against spike *increased* up to 8 months after infection. science.org/doi/10.1126/sc… 67/ 

So, it’s complicated, and still hard to know which mode of acquiring immunity (NI or VI) will be superior in long term (>1 year) given effects on cellular immunity, and also the now-common practice of offering third doses (let alone new boosters optimized to future variants). 68/
Finally, a host of studies shows that vaccinating those who are previously infected offers further benefits. In addition to studies cited higher in this thread, we also have evidence from other studies. Here are just a few examples, below. 69/
Kentucky residents with previous infections who were unvaccinated had 2.34 times the odds of reinfection (OR = 2.34; 95% CI = 1.58–3.47) compared with those who were also fully vaccinated (i.e., NI+VI > NI). cdc.gov/mmwr/volumes/7… 70/
One dose of an mRNA vaccine among those previously infected is probably all that is needed to derive benefit. science.org/doi/10.1126/sc… 71/
A single dose of mRNA vaccine really seems to help enhance immune response among those who were previously infected (i.e., NI+VI > NI). science.org/doi/10.1126/sc… 72/ 

In short, it’s wisest, even if you have had COVID-19, but especially if you are older or had a mild illness, to get vaccinated with an mRNA vaccine.
Those with a combination of natural immunity & vaccination are likely in best position to fight new variants, eg, omicron etc. 73/
Those with a combination of natural immunity & vaccination are likely in best position to fight new variants, eg, omicron etc. 73/
I have no political agenda here. Natural immunity is clearly not bad! But this topic has become politicized, in part because anti-vaxers want to be able to reject the claim that vaccines help a lot, including also among those with natural immunity. 74/
This has been my longest COVID-19 thread to date (and I started doing this in February of 2020). The literature on this topic – and so many COVID topics – is enormous and growing. As it grows, and as the pandemic changes, I reserve the right to update my opinion. :-) 75/
Some desiderata and new citations to follow up this long thread on the relative protection offered by infection-acquired immunity (or ‘natural immunity’ – NI) versus vaccine-acquired immunity (VI) for COVID-19, including with respect to omicron. Other updates may follow. 76/
First, there are a number of reasons that, regardless of the actual quantitative difference between NI and VI, and regardless of circumstances, we might still wish to encourage or even require vaccination as a broad policy. 77/
As noted above, properly testing everyone to prove NI might not be easy to implement, and it might be logistically easier to simply try to vaccinate everyone. 78/
Moreover, vaccinating the already immune is good for them individually (it enhances immunity, as many of the very same studies anti-vaxxers cite – and included above and below in this thread – show). That is: NI + VI > NI 79/
Finally, from public health point of view, we do not want to encourage people to affirmative seek out infection (ironically, ‘in order to become immune’). That makes little sense. Of course, this late in the pandemic, most of those with NI just got it without actually trying. 80/
So a policy of “everyone should be vaccinated” can be rational from many public health points of view. 81/
Now, another (fantastic) study from Israel appeared on December 5, 2021 showing material superiority of infection-induced immunity (or ‘natural immunity’ – NI) compared to vaccine-induced immunity (VI). medrxiv.org/content/10.110… 82/
A total of 5.7M Israelis were followed from August 2020, through February 2021 when vaccination began in earnest in Israel, and until September 30, 2021. This population was exposed to many SARS2 variants including delta. 83/
These 5.7M people were divided into 5 groups in this terrific study:
Recovered (previously infected ppl)
Recovered then Vaccinated
Vaccinated then Recovered (two doses and later infected)
Vaccinated (ppl w 2 doses who had not been infected)
Booster (ppl with 3 doses)
84/
Recovered (previously infected ppl)
Recovered then Vaccinated
Vaccinated then Recovered (two doses and later infected)
Vaccinated (ppl w 2 doses who had not been infected)
Booster (ppl with 3 doses)
84/
At 6-8 months post-exposure, the adjusted *infection rate* per 100,000 person-days is:
Recovered: 14.8
Vaccinated: 88.9
Recovered then vaccinated: 11.6
So, NI>VI. And, again, NI + VI > NI 85/
Recovered: 14.8
Vaccinated: 88.9
Recovered then vaccinated: 11.6
So, NI>VI. And, again, NI + VI > NI 85/

The story is similar (though counts are low) with *serious illness*, meaning that rates of severe disease for those >60 “were 0.6 per 100,000 person-days in Recovered; 0.5 in Recovered then Vaccinated; 1.1 in Vaccinated then Recovered; 4.6 in Vaccinated; and 0.4 for Booster” 86/
This means that, among the elderly, those in the boosted category (three shots) had slightly *lower* COVID19 mortality than those in the recovered category. So, for them, VI may be slightly higher than NI (again, without having had to run the prior ~1% chance of death!). 87/
There are some statistical details not worthy of tweets here, including whether: standard errors were adjusted for fact people could contribute days to more than one cohort; negative binomial regression could have been better; better washout periods could have been used, etc. 88/
So, the bottom line in this very well conducted study (medrxiv.org/content/10.110…), is that, overall, NI is better than VI. And NI + VI is superior to either NI or VI alone. But VI > NI for elderly people with boosters. 89/
What can we say about the relative strength of NI and VI against the newest variant of concern, omicron? A study out on December 21, 2021 (yesterday) via JM Carreno & @florian_krammer et al finds that, in vitro, boosted individuals have good protection medrxiv.org/content/10.110… 90/
The study investigated the in vitro neutralizing and binding activity of sera from N=85 convalescent, mRNA double vaccinated, mRNA boosted, and convalescent boosted or double-boosted individuals against the original, omicron, and other SARS2 variants. 91/
Neutralizing activity of sera from convalescent and double-jabbed ppl was undetectable or very low against omicron.
But neutralizing activity of sera from individuals who had been exposed to spike 3-4 times (eg, boosted ppl) was maintained, albeit at strongly reduced levels. 92/
But neutralizing activity of sera from individuals who had been exposed to spike 3-4 times (eg, boosted ppl) was maintained, albeit at strongly reduced levels. 92/
So, this fine (in vitro) study suggests that (over at least a short time horizon after vaccination) those with three doses of an mRNA vaccine should fare better against omicron than those with prior infection. Infection-induced immunity is not as good. That is, VI > NI, here. 93/
And another in vitro study posted yesterday , December 21, 2021, reached a similar conclusion regarding thrice-jabbed people and omicron (biorxiv.org/content/10.110…). It found that “three doses of mRNA vaccination rescues neutralisation in the short term.” 94/
More evidence re relative strength of vaccine-mediated & infection-mediated immunity to COVID-19 continues to amass, incl this great @CDCgov study yesterday (1/19/22): cdc.gov/mmwr/volumes/7…. It shows better immunity against re-infection in those surviving prior infection... 95/
The study covers a period of time for original Wuhan and delta strains of virus, from May-Nov 2021 (in CA & NY). Subjects mostly did *not* have boosters. Against original strain, vaccine-mediated immunity was better able to protect against infection & hospitalization. VI>NI 96/
But by delta wave, those who had survived prior COVID19 infection fared better (in terms of immune protection) than those who were vaccinated. NI>VI. To be clear, the vaccinated here were mostly unboosted, & (again) to get "natural" immunity, one must first run risk of death. 97/
Still, this terrific @CDCgov study (cdc.gov/mmwr/volumes/7…) shows that, by delta wave, those who had run the risk of death and survived infection had very substantial immunity against serious illness from reinfection. 98/ 

In Oct 2021, compared with hospitalization rate in unvaccinated ppl without prior COVID19, hospitalization was 19.8-fold lower in vaccinated ppl without prior COVID; 55.3-fold lower in unvaccinated ppl with prior COVID; & 57.5-fold lower in vaccinated ppl with prior COVID. 99/
Note that this study shows benefit of having been vaccinated among those who also had been infected. NI+VI > NI 100/
The story about whether infection or vaccination confers superior immunity against serious COVID19 upon re-exposure to SARS-CoV-2 continues to evolve, and will depend upon prevalent strains and nature of vaccination (eg boosters). Situation with omicron is still not clear. 101/
• • •
Missing some Tweet in this thread? You can try to
force a refresh













