
1/ There are a lot of takes that this omicron wave will bring us closer to “normal” in 2022 when COVID will become endemic and be “just like the flu.” A comparison with historical flu seasons shows just how far away this really is and how much longer we may need to go. 🧵
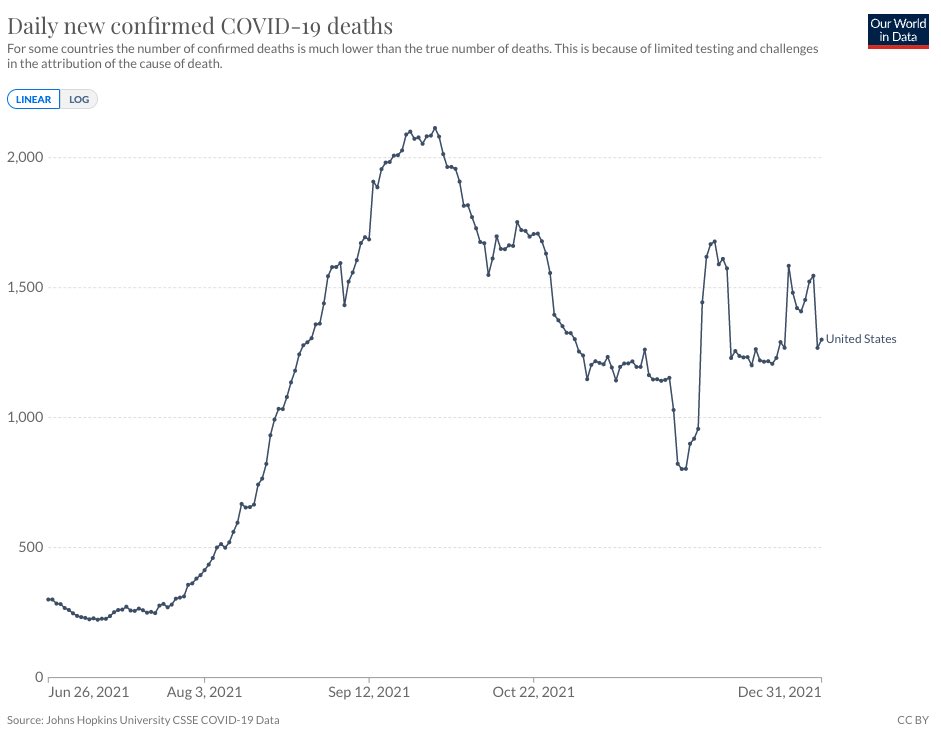
2/ The key societal question is what level of mortality & morbidity do we accept from COVID in the long run. If influenza is the right analogue, then this chart shows that COVID has broken well beyond the baseline and “epidemic” threshold of mortality of prior flu seasons. 

3/ “Just like the flu,” you say?
Let’s drill into some US data:
* 11,707 weekly PIC (pneumo, influenza, COVID) deaths since Labor Day
* At the peak of Delta, ~18,000 weekly PIC deaths
This is 3-5x our pre-COVID flu baseline (~3,500 weekly deaths).
cdc.gov/flu/weekly/wee…
Let’s drill into some US data:
* 11,707 weekly PIC (pneumo, influenza, COVID) deaths since Labor Day
* At the peak of Delta, ~18,000 weekly PIC deaths
This is 3-5x our pre-COVID flu baseline (~3,500 weekly deaths).
cdc.gov/flu/weekly/wee…
4/ The mortality rate could be viewed as a proxy for all sorts of decisions that individuals, companies, policymakers make to gauge how dangerous COVID is and what structural changes we need to make to protect lives.
5/ My heuristic is that things will feel “normal” when the mortality rate is <500 deaths per day (i.e., the pre-COVID flu baseline), which coincidentally was the rate last summer when we declared “independence” from COVID. 
6/ A “new normal” of 500 deaths/day from endemic COVID would be a non-trivial loss to bear “forever” — this loss of life implies a structural change in our healthcare system and economy (@$10 M “value per statistical life”, this equates to a $1.8 trillion annual loss for the US).
7/ What will it take to reduce the mortality rate by >50-70%?
* Omicron ends up being less severe than Delta (yes, but…)
* The vax/booster rate increases materially (not happening fast enough)
* Oral therapies live up to their promise in real world (jury’s out)
* Omicron ends up being less severe than Delta (yes, but…)
* The vax/booster rate increases materially (not happening fast enough)
* Oral therapies live up to their promise in real world (jury’s out)
8/ While omicron appears to be less severe on a per case basis, the sheer volume of new cases right now means the overall pool of people susceptible is much larger. Net-net, a lot of people are still dying from a “milder” variant. 

9/ Omicron has not yet fully spread to the older, sicker segment of the population and the worst could be yet to come with more time.
cnbc.com/2021/12/29/cov…
cnbc.com/2021/12/29/cov…
10/ I already wrote about Paxlovid and why it may not be the silver bullet:
https://twitter.com/cha_myoung/status/1476080634158219264
11/ And remember, we have already had remdesivir for a while now in our toolkit, which is comparable in efficacy to Paxlovid.
https://twitter.com/antonioregalado/status/1477360207630114838
12/ Even if we manage to get the death rate down, the volatility of COVID surges must be lower for us to treat COVID as an endemic phenomenon. Each new variant has brought with it a surge in cases and hospitalizations that has stressed our healthcare system.
13/ The omicron “flash flood” phenomenon compounds the volatility with the sheer number of people who are getting sick at the same time — even when they aren’t sick enough to be hospitalized — a “soft lockdown” in effect. theatlantic.com/health/archive…
14/ Estimates of 60% of people getting sick from omicron (140 M people) in the next few months would be 4-5x the number of people who get sick with flu in a “normal” year.
usatoday.com/story/news/hea…
usatoday.com/story/news/hea…
15/ The trillion-dollar question is whether the omicron wave will induce durable and strong immunity. After all of the data we have seen on waning immunity (both vaccine-based and natural), my bet is the immunity will be short-lived and/or weak.
https://twitter.com/bob_wachter/status/1477334569120534528
16/ There are even signs of waning immunity in those who have so-called “super-immunity”
nature.com/articles/d4158…
nature.com/articles/d4158…
17/ None of the above takes into account the unknown morbidity that comes from a COVID infection (or repeated infections over time). It would radically change the game if the risk of long COVID from omicron was found to be material.
18/ It is too late to impact this current wave, but we should be doing everything in our power over the next year to get ready for a similar (or more devastating) variant next fall.
• • •
Missing some Tweet in this thread? You can try to
force a refresh












