#JanuAIRWAY Day 4. Airway Investigations. 2 broad categories we can use to round out our airway assessment; flow/volume-based lung function tests & imaging techniques. They vary in their usage and usefulness. Here's some #OnePagers #FOAMed on Spirometry and Flow-volume loops 1/17 



Spirometry (literally ‘measuring breath’) and flow-volume loops give us information on the mechanics of ventilation. They can be helpful in a more global assessment of respiratory function, but are less helpful in acute airway management.
#JanuAIRWAY #FOAMed 2/17

#JanuAIRWAY #FOAMed 2/17


Diffusing Capacity / Transfer factor can augment lung function tests and give us info about alveolar diffusion and alveolar thickness. Again, helpful in global assessment, but less helpful acutely. Here’s another #OnePager covering the theory and the practice
#JanuAIRWAY 3/17
#JanuAIRWAY 3/17

Imaging techniques – these can be incredibly useful in peri-operative management. Two main types: radiological (CT and/or USS) and endoscopic techniques (we’ll cover USS & nasendoscopy more later this month). Here’s a #OnePager on the essentials of airway CT #JanuAIRWAY 4/17 

Key information you want is:
1) Is an airway abnormality present?
2) If so what kind – usually compression/stenosis
a. Lesion location and extent?
b. Maximal airway diameter?
c. Airway displacement?
d. Other structures involved/in the way (eg blood vessels)?
#JanuAIRWAY 5/17
1) Is an airway abnormality present?
2) If so what kind – usually compression/stenosis
a. Lesion location and extent?
b. Maximal airway diameter?
c. Airway displacement?
d. Other structures involved/in the way (eg blood vessels)?
#JanuAIRWAY 5/17
Here are some papers / links that you might find interesting: -
a. academic.oup.com/bjaed/article/…
b. sciencedirect.com/science/articl…
c. bjanaesthesia.org.uk/article/S0007-…
If you have any others of interest, tweet them to us for inclusion next time!
#JanuAIRWAY 6/17
a. academic.oup.com/bjaed/article/…
b. sciencedirect.com/science/articl…
c. bjanaesthesia.org.uk/article/S0007-…
If you have any others of interest, tweet them to us for inclusion next time!
#JanuAIRWAY 6/17
What about Airway Ultrasound? It’s an amazing skill in managing airways. It’s pretty simple. Check out Michael Seltz Kristensen's work – undisputed master of airway ultrasound. Here’s a #OnePager on the basics
#JanuAIRWAY 7/17
#JanuAIRWAY 7/17

Indications?
1) Assessment – tracheostomy, fasting status & pneumothorax
2) Intervention – cricothyroidotomy / regional anaesthesia (superior laryngeal nerve)
For gastric contents USS check out @elboghdadly , Wojcikiewicz & Perlas’
work bjaed.org/article/S2058-…
#JanuAIRWAY 8/17
1) Assessment – tracheostomy, fasting status & pneumothorax
2) Intervention – cricothyroidotomy / regional anaesthesia (superior laryngeal nerve)
For gastric contents USS check out @elboghdadly , Wojcikiewicz & Perlas’
work bjaed.org/article/S2058-…
#JanuAIRWAY 8/17
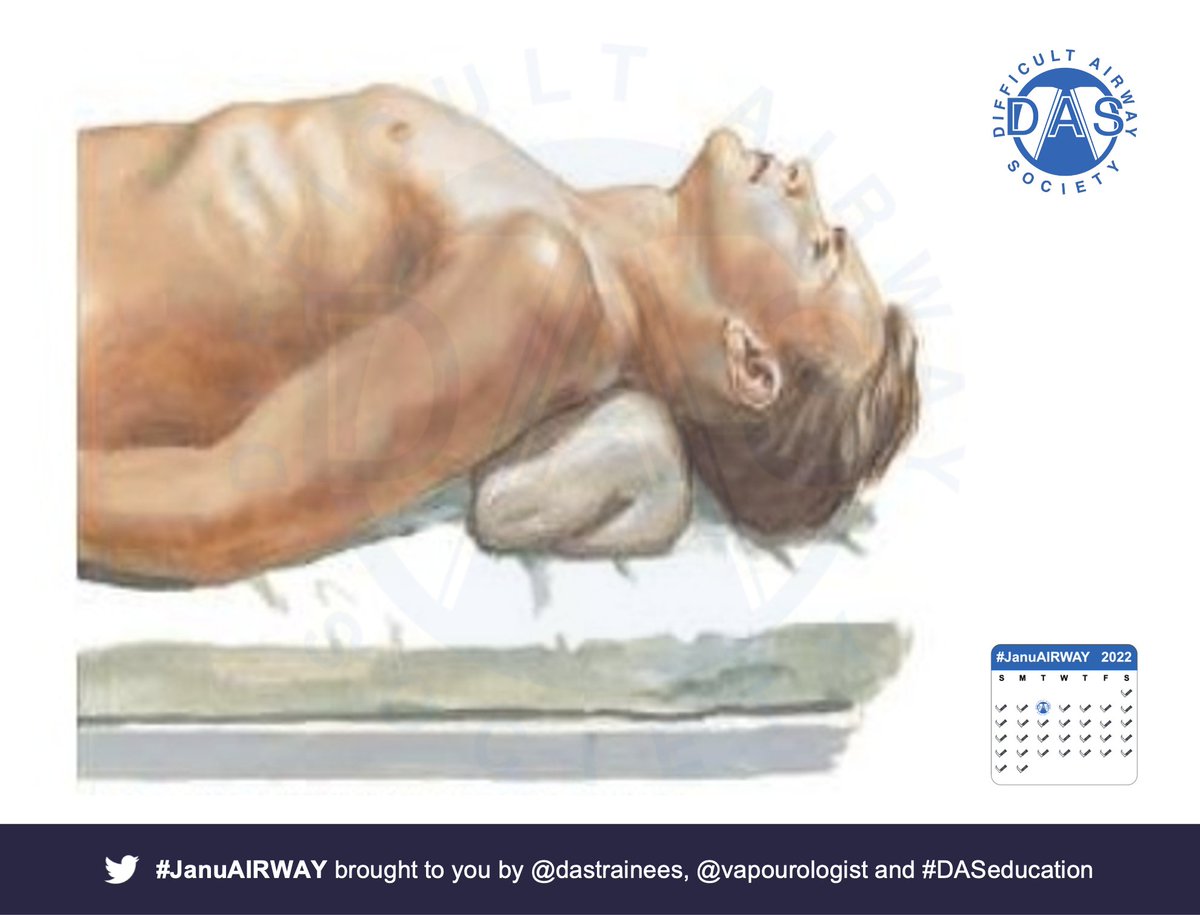
Today we’ll focus on the transverse views for cricothyroidotomy #POCUS. Start by getting the patient in the position, in which you would perform a cricothyroidotomy/tracheostomy – consider a bag of fluid under the shoulders
#JanuAIRWAY 9/17
#JanuAIRWAY 9/17
Linear probe / transverse orientation. Start with probe on neck under chin. Scan inferiorly until you see the thyroid cartilage – triangular or inverted V-appearance between strap muscles (angle of thyroid cartilage is more acute in males) #FOAMed #POCUS
#JanuAIRWAY 10/17
#JanuAIRWAY 10/17

Scan caudally looking for air-mucosa interface - very bright hyperechoic white line - represents beginning of tracheal lumen at cricothyroid membrane– hence target for cricothyroidotomy (reverberation artefact is below in tracheal lumen beneath) #POCUS #FOAMed
#JanuAIRWAY 11/17
#JanuAIRWAY 11/17

You can mark the position of the cricothyroid membrane at this level with a pen on either side of the probe (left & right, top & bottom) #POCUS #FOAMed
#JanuAIRWAY 12/17
#JanuAIRWAY 12/17
Continuing caudally the cricoid cartilage comes into view as a hypoechoic inverted U or horse-shoe shape with the Air-Mucosa Interface below. ) #POCUS #FOAMed
#JanuAIRWAY 13/17
#JanuAIRWAY 13/17

The tracheal rings will come into view as hypoechoic ring-like shapes with Air-Muscosa Interface below and Thyroid gland above and to either side – useful to know it’s location and vascularity before percutaneous tracheostomy!) #POCUS #FOAMed
#JanuAIRWAY 14/17
#JanuAIRWAY 14/17

Longitudinal / parasagittal views along trachea, air-mucosa interface = long white line, cartilages appear as hypoechoic ovals – Kristensen calls them a ‘string of pearls’ – they look a bit like coffee beans! Use Touhy needle to identify level. #POCUS #FOAMed
#JanuAIRWAY 15/17
#JanuAIRWAY 15/17

Here's some papers/links you might find interesting:
a. sciencedirect.com/science/articl…
b. pubmed.ncbi.nlm.nih.gov/20645953/
c. pubmed.ncbi.nlm.nih.gov/21423020/
d. airwaymanagement.dk/pearls
e. bjaed.org/article/S2058-…
Tweet us any others of interest for inclusion next time!
#JanuAIRWAY 16/17
a. sciencedirect.com/science/articl…
b. pubmed.ncbi.nlm.nih.gov/20645953/
c. pubmed.ncbi.nlm.nih.gov/21423020/
d. airwaymanagement.dk/pearls
e. bjaed.org/article/S2058-…
Tweet us any others of interest for inclusion next time!
#JanuAIRWAY 16/17
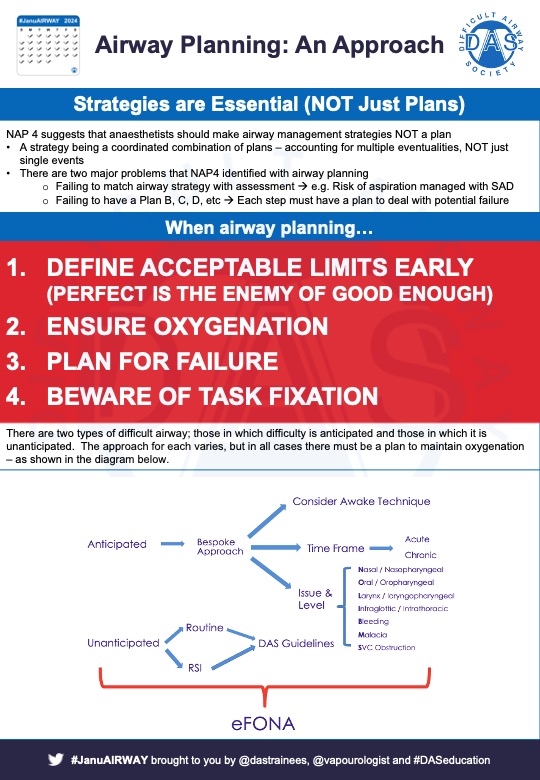
Hope that helps. Tomorrow we'll look at planning/strategising in airway management
*Disclaimer: Inclusion of content (equipment, techniques and scoring systems etc.) in #JanuAIRWAY does not constitute DAS endorsement 17/17
*Disclaimer: Inclusion of content (equipment, techniques and scoring systems etc.) in #JanuAIRWAY does not constitute DAS endorsement 17/17
• • •
Missing some Tweet in this thread? You can try to
force a refresh