1/ @ZekeEmanuel @mtosterholm @llborio @RickABright @drdavidmichaels published 3 Viewpoints in
@JAMA_current on an updated national strategy for controlling COVID.
1st in the series:
A National Strategy for the “New Normal” of Life With COVID
jamanetwork.com/journals/jama/…
@JAMA_current on an updated national strategy for controlling COVID.
1st in the series:
A National Strategy for the “New Normal” of Life With COVID
jamanetwork.com/journals/jama/…
2/ We've got to set realistic goals: to flatten the curve, and to suppress COVID hospitalizations & deaths.
Our health system is buckling under the weight of COVID. This is not sustainable.
The good news is that measures to control SARS-CoV-2 will also control influenza & RSV.
Our health system is buckling under the weight of COVID. This is not sustainable.
The good news is that measures to control SARS-CoV-2 will also control influenza & RSV.

3/ Masking😷, ventilation🪟 & air filtration will control COVID, influenza, RSV, & other viral respiratory illnesses.
Vaccines💉, rapid antigen tests & antiviral drugs💊 can also help reduce influenza transmission, cases, hospitalizations & deaths.
Vaccines💉, rapid antigen tests & antiviral drugs💊 can also help reduce influenza transmission, cases, hospitalizations & deaths.
4/ Our goal should be to control hospitalizations & deaths from ALL viral respiratory illnesses.
What level of hospitalizations & deaths from viral respiratory illnesses should we aim for?
We can start with what the public, health system & the economy have accepted in the past.
What level of hospitalizations & deaths from viral respiratory illnesses should we aim for?
We can start with what the public, health system & the economy have accepted in the past.
5/ We don't shut down the economy or society for bad flu years.
Using prior peak influenza & RSV years, we've been willing to accept a risk threshold of
~35K hospitalizations per week
& 3K deaths per week
from ALL viral respiratory illnesses.
Using prior peak influenza & RSV years, we've been willing to accept a risk threshold of
~35K hospitalizations per week
& 3K deaths per week
from ALL viral respiratory illnesses.
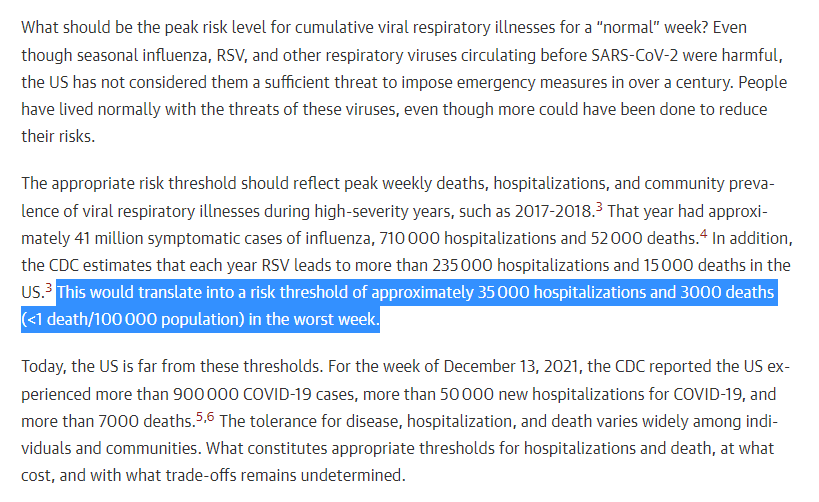
6/ We're currently at
over 16K COVID hospitalizations per week & rising
covid.cdc.gov/covid-data-tra…
over 1200 COVID deaths per week & rising
covid.cdc.gov/covid-data-tra…
on top of influenza & RSV hospitalizations/deaths.
over 16K COVID hospitalizations per week & rising
covid.cdc.gov/covid-data-tra…
over 1200 COVID deaths per week & rising
covid.cdc.gov/covid-data-tra…
on top of influenza & RSV hospitalizations/deaths.
7/ Risk thresholds based on hospitalizations & deaths from ALL viral respiratory illnesses would allow health departments to recommend emergency mitigation & other measures as needed.
And they're a way of measuring the success of viral respiratory illness control measures.
And they're a way of measuring the success of viral respiratory illness control measures.
8/ Health systems can use risk thresholds based on hospitalizations to plan & surge bed and workforce capacity.
Here's one example of such a dashboard:
Here's one example of such a dashboard:
https://twitter.com/jeremyfaust/status/1479244541127446531?s=20by @jeremyfaust @BillHanage @bhrenton
9/ What is the right risk threshold for hospitalizations & deaths from ALL viral respiratory illnesses moving forward?
Prior numbers are a place to start.
Different communities will have different tolerance for risk.
Ditto for hospitals & health systems.
Prior numbers are a place to start.
Different communities will have different tolerance for risk.
Ditto for hospitals & health systems.
10/ In addition to agreeing on the goals of our COVID control strategy,
we've got to rebuild public health.
we've got to rebuild public health.
11/ Need comprehensive, digital, real-time, integrated public health data infrastructure:
- national, state, local health dept data
- health care system data
- lab data, including academic & commercial
- environmental surveillance data (air, water, wastewater)
- national, state, local health dept data
- health care system data
- lab data, including academic & commercial
- environmental surveillance data (air, water, wastewater)
12/ Need public health workforce:
- (re)building capacity, empowering & funding health depts
khn.org/news/tag/under…
- community health workers
- school nurses
Also need MORE healthcare workers in hospitals & more flexibility to move them around during emergencies as needed.
- (re)building capacity, empowering & funding health depts
khn.org/news/tag/under…
- community health workers
- school nurses
Also need MORE healthcare workers in hospitals & more flexibility to move them around during emergencies as needed.

13/ Need to rebuild trust in public health institutions,
the belief that we're all in this together,
& the belief that we should & can work together in service of public health.
the belief that we're all in this together,
& the belief that we should & can work together in service of public health.
14/ This starts with public health systems that respond promptly, visibly, effectively in real-time to public health crises & to the needs of the community.
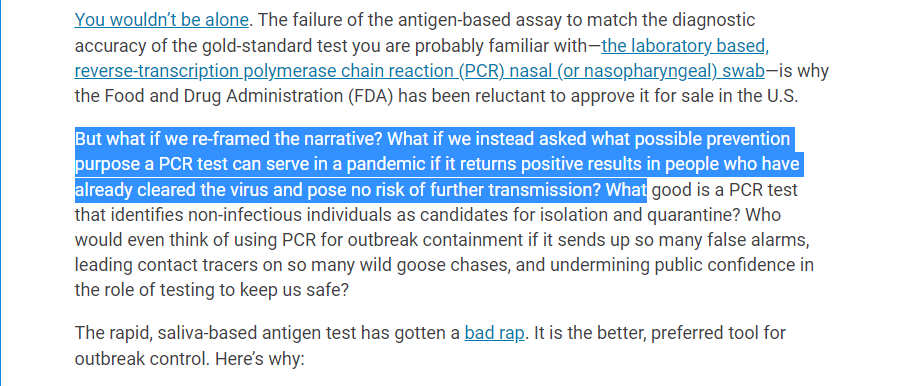
16/ Testing was a mess early in the pandemic:
justhumanproductions.org/podcasts/e2-th…
We still don't have widely available, cheap/free testing.
Why? More on that here 👇🏾👇🏾👇🏾
justhumanproductions.org/podcasts/e2-th…
We still don't have widely available, cheap/free testing.
Why? More on that here 👇🏾👇🏾👇🏾
https://twitter.com/celinegounder/status/1477737116004143107?s=20
17/ We're doing dramatically more genomic surveillance in the U.S. than we were doing in early 2021, but there's still much room for improvement.
We've been calling for this for months:
We've been calling for this for months:
https://twitter.com/celinegounder/status/1364588805924257797?s=20
18/ We were too slow to recognize the importance of aerosol transmission of SARS-CoV-2.
I discussed this with @MIT's Lydia Bourouiba & @rkhamsi in MARCH 2020:
justhumanproductions.org/podcasts/a-fal…
I discussed this with @MIT's Lydia Bourouiba & @rkhamsi in MARCH 2020:
justhumanproductions.org/podcasts/a-fal…
19/ This led to incorrect, delayed & highly confusing recommendations on masking, wearing high-quality respirators & improving ventilation.
With a variant as infectious as Omicron, you should up your mask game.
Wear an N95, KN95, or KF94 (buy here: projectn95.org).
With a variant as infectious as Omicron, you should up your mask game.
Wear an N95, KN95, or KF94 (buy here: projectn95.org).
20/ Congress has allocated HUNDREDS OF BILLIONS of dollars to improve ventilation & air filtration in K-12 schools.
We're squandering this once in a lifetime opportunity:
thehill.com/opinion/educat… with @j_g_allen
We're squandering this once in a lifetime opportunity:
thehill.com/opinion/educat… with @j_g_allen

21/ We should be upgrading indoor ventilation & air filtration to reduce the burden of ALL viral respiratory illnesses, including COVID.
This is a win-win:
A win for public health.
An opportunity for public-private partnership.
An opportunity to create good paying HVAC jobs.
This is a win-win:
A win for public health.
An opportunity for public-private partnership.
An opportunity to create good paying HVAC jobs.
22/ The new HHS website for ordering free rapid antigen testing should also offer free high-quality masks.
washingtonpost.com/nation/2022/01…
washingtonpost.com/nation/2022/01…
23/ Meanwhile, NYC is installing vending machines with free naloxone, clean syringes, toiletries & safe-sex kits.
Why not masks and rapid antigen tests, too?
nytimes.com/2022/01/08/nyr…
Why not masks and rapid antigen tests, too?
nytimes.com/2022/01/08/nyr…
24/ 3rd Viewpoint in the series:
jamanetwork.com/journals/jama/…
by @llborio @RickABright @ZekeEmanuel
jamanetwork.com/journals/jama/…
by @llborio @RickABright @ZekeEmanuel
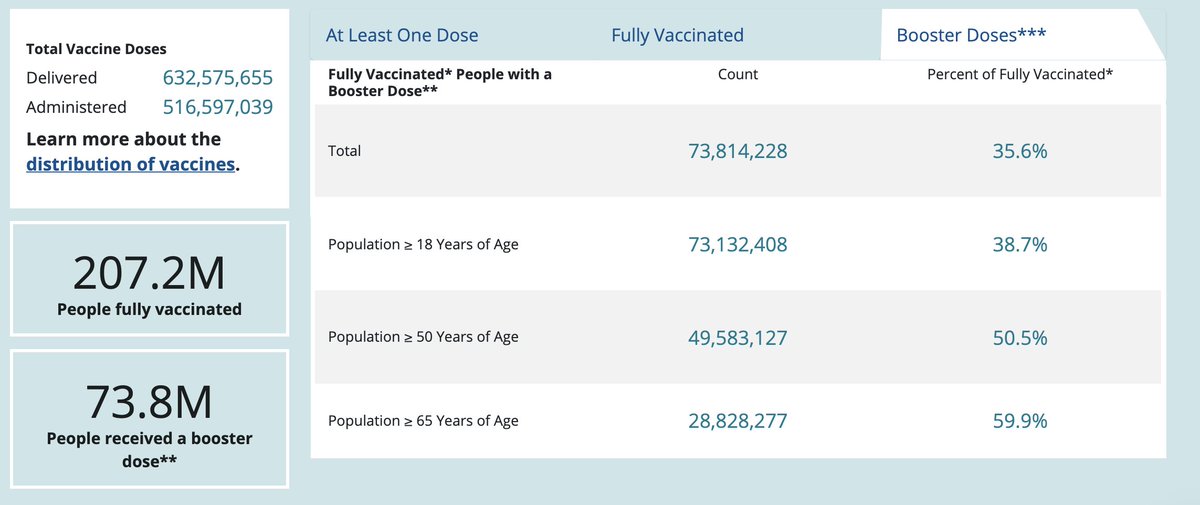
29/ We need to give a lot more boosters, especially to Americans over 50, who are at much higher risk for hospitalization and death from COVID: 
30/ Depending on our goals, how immunity evolves over time after vaccination &/or infection, and how the virus mutates over time, our vaccine regimens will also evolve over time.
nytimes.com/2021/08/09/opi…
with Drs. John Moore & @CarlosdelRio7
nytimes.com/2021/08/09/opi…
with Drs. John Moore & @CarlosdelRio7
31/ Some vulnerable populations, especially the elderly🧓🏿, highly immunocompromised, & residents of long-term care facilities
& people in some occupations, e.g. healthcare🏥🩺, caregiving👩🏾⚕️🧑🏻⚕️
may need annual boosters💉💉💉.
But not necessarily the general public.
& people in some occupations, e.g. healthcare🏥🩺, caregiving👩🏾⚕️🧑🏻⚕️
may need annual boosters💉💉💉.
But not necessarily the general public.
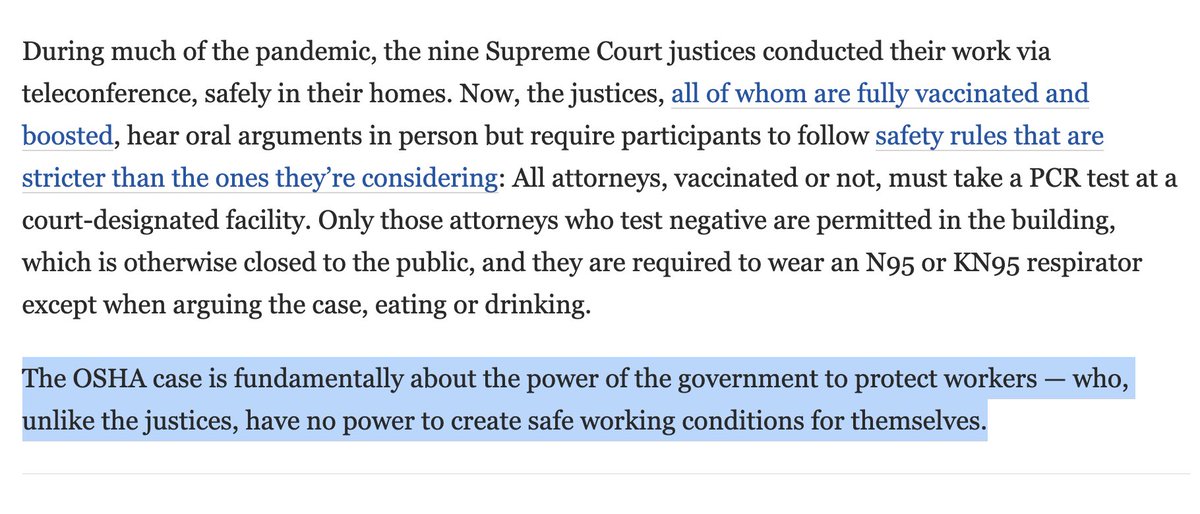
33/ It looks like the Supreme Court may uphold vaccination requirements for staff at health facilities accepting Medicare/Medicaid funding
BUT NOT
@OSHA_DOL rule on vaccination or testing for employers with 100+ workers.
nytimes.com/2022/01/07/us/…
BUT NOT
@OSHA_DOL rule on vaccination or testing for employers with 100+ workers.
nytimes.com/2022/01/07/us/…
34/ And that means we're unlikely to hit 90% vaccination coverage in the U.S. without other strategies.
Some other possibilities:
- Mandates (e.g. school, travel, large venues, indoor restaurants/bars/gyms/salons/spas)
- Incentives
- Voluntary
Some other possibilities:
- Mandates (e.g. school, travel, large venues, indoor restaurants/bars/gyms/salons/spas)
- Incentives
- Voluntary
35/ The longer it takes us to⬆️COVID vaccination coverage, the longer it will take to reach endemicity and a stable steady-state with the SARS-CoV-2 virus.
36/ In the future, we may need to update our vaccines for new variants.
We should continue optimizing vaccine regimens:
- longer delay between 1st & 2nd doses
- heterologous mix & match regimens
We should continue optimizing vaccine regimens:
- longer delay between 1st & 2nd doses
- heterologous mix & match regimens
37/ We should work on developing:
- mucosal vaccines to improve immunity in the upper airway (i.e. nose👃🏾, mouth👄, throat)
- microarray skin patches to deliver vaccine more slowly over time
- pan-sarbecovirus vaccines
- mucosal vaccines to improve immunity in the upper airway (i.e. nose👃🏾, mouth👄, throat)
- microarray skin patches to deliver vaccine more slowly over time
- pan-sarbecovirus vaccines
38/ We need 21st-century vaccine verification systems that protect privacy & equity.
justhumanproductions.org/podcasts/s1e77…
justhumanproductions.org/podcasts/s1e77…
39/ And we need to ensure global vaccine equity,
including regional manufacturing self-sufficiency.
justhumanproductions.org/podcasts/s1e76…
including regional manufacturing self-sufficiency.
justhumanproductions.org/podcasts/s1e76…
40/ In the hospital, we mostly use dexamethasone & remdesivir to treat COVID patients.
We need better-targeted immunomodulators for late-stage disease.
We need better-targeted immunomodulators for late-stage disease.
41/ In the out-patient setting, monoclonal antibodies work well when given early, but Omicron is resistant to our currently available monoclonal antibodies except sotrovimab.
endpts.com/us-ships-out-a…
endpts.com/us-ships-out-a…
42/ New oral antiviral drugs (Pfizer's Paxlovid & Merck's monulpiravir) are on the way, but will be will have no impact without a foundation of cheap, rapid, widely available/accessible testing & treatment:
https://twitter.com/celinegounder/status/1456993934069149705?s=20
43/ We need to monitor for emerging resistance to Paxlovid and monulpiravir.
We need to be developing additional antivirals.
And we need to study the use of antivirals for:
- pre- & post-exposure prophylaxis
- prevention & treatment of long COVID
We need to be developing additional antivirals.
And we need to study the use of antivirals for:
- pre- & post-exposure prophylaxis
- prevention & treatment of long COVID
44/ Yesterday, I joined @MSNBC's @AliVelshi to discuss the 3 @JAMA_current Viewpoints outlining a new national COVID strategy
jamanetwork.com/journals/jama/…
by @ZekeEmanuel @mtosterholm @llborio @RickABright @drdavidmichaels & me:
jamanetwork.com/journals/jama/…
by @ZekeEmanuel @mtosterholm @llborio @RickABright @drdavidmichaels & me:
46/ Join me & @ZekeEmanuel tomorrow on @NBC's @MeetThePress with @ChuckTodd
to hear more about the new national COVID strategy @ZekeEmanuel, @mtosterholm, @llborio, @RickABright, @drdavidmichaels & I outlined in @JAMA_current
this week.
jamanetwork.com/journals/jama/…
to hear more about the new national COVID strategy @ZekeEmanuel, @mtosterholm, @llborio, @RickABright, @drdavidmichaels & I outlined in @JAMA_current
this week.
jamanetwork.com/journals/jama/…
• • •
Missing some Tweet in this thread? You can try to
force a refresh